Abstract
Background: In pediatric B-precursor acute lymphoblastic leukemia (ALL), hyperdiploidy (51 to 65 chromosomes and/or DNA index > 1.16) comprises approximately 25% of cases and is associated with a favorable prognosis.
Aim: To evaluate the clinical and relapse characteristics of children with hyperdiploid (HY) ALL treated at Children’s Hospital of Michigan from 1991 to 2002.
Methodology: Children were treated per several successive Pediatric Oncology Group ALL studies. Data was obtained by retrospective chart review. Study end-points were "relapse" or "death" whichever came first. Univariate and multivariate analysis was performed to study the association of various clinical and biological factors on outcome. Survival curves were drawn using Log-rank test.
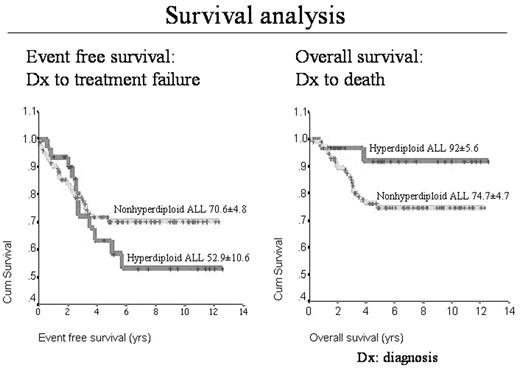
Results: 139 children diagnosed with ALL were included in the study: 31 (22%) HY-ALL; 108 (88%) non-HY-ALL (Table). In HY-ALL, 11(35%) relapsed: 3 (27%) isolated hematopoietic (HEM); 8 (73%) extra-medullary (EM) [TESTES: 4; TESTIS+HEM: 1; CNS+HEM: 3]. Two (18%) relapsed while on treatment. Non-HY-ALL relapses occurred in 25 (23%): HEM 16 (64%); EM 9 (46%) [TESTIS: 1; TESTIS+HEM: 1; CNS: 6; CNS+HEM: 1]. Thus, HY-ALL children were predisposed to EM involvement at relapse compared to non-HY-ALL (p<0.02; OR 3.82; 95%CI 1.37 to 10.7). Twenty percent (4/20) of boys with HY-ALL experienced testicular relapse as opposed to 3% (2/58) in non-HY-ALL (p 0.06; OR 7.0; 95% CI 1.35 to 35.65). For the HY-ALL group, age >10 years and Caucasian race were associated with poor EFS (p<0.03). Within the HY-ALL group, there was no significant difference in cumulative methotrexate and 6-mercaptopurine doses between patients who relapsed and patients who remained in remission. Respective 10 year event-free survival for the HY-ALL and non-HY-ALL cohort was 52.9± 10.6% and 70.6±4.8% (p 0.12) and overall survival (OS) for HY-ALL and non-HY-ALL groups was 92±5.6 and 74±4.7, (p 0.14). Relapse related mortality was 18% (2/11) for HY-ALL and 80% (20/25) for non-HY-ALL (p 0.002; OR 0.06; 95% CI 0.01 to 0.32).
Conclusion: Relapses in HY-ALL predominantly involved EM sites. Despite relapses, HY-ALL cases remained sensitive to salvage therapy with a high OS. This suggests that the basis of relapse may differ between HY-ALL and non-HY-ALL cases and the relationship of drug resistance with relapse. Older children (>10 yr) with HY-ALL may require more intensive treatment and monitoring of sanctuary sites to prevent treatment failures.
Patient Characterisitcs at Diagnosis
| Patient characterisitcs . | Hyperdiploid ALL (n=31) . | Non-Hyperdiploid ALL (n=108) . |
|---|---|---|
| CAUC: Caucasian; AA: African American; O: Other | ||
| Median age (yrs) | 3.9 (1.3–16.0) | 5.8 (3.0–17.0) |
| Race: CAUC/AA/O | 21(69%)/ 6(19%)/ 4(12%) | 66(61%)/ 28(26%)/ 14(12%) |
| Age>10 yr | 5 (16%) | 13 (12%) |
| Male:Female | 20 (65%):11(35%) | 58 (54%):50(46%) |
| Median follow up (yrs) | 5.9 ± 4.0 | 5.3 ±3.4 |
| Events | 11 (35%) | 30 (28%) |
| Patient characterisitcs . | Hyperdiploid ALL (n=31) . | Non-Hyperdiploid ALL (n=108) . |
|---|---|---|
| CAUC: Caucasian; AA: African American; O: Other | ||
| Median age (yrs) | 3.9 (1.3–16.0) | 5.8 (3.0–17.0) |
| Race: CAUC/AA/O | 21(69%)/ 6(19%)/ 4(12%) | 66(61%)/ 28(26%)/ 14(12%) |
| Age>10 yr | 5 (16%) | 13 (12%) |
| Male:Female | 20 (65%):11(35%) | 58 (54%):50(46%) |
| Median follow up (yrs) | 5.9 ± 4.0 | 5.3 ±3.4 |
| Events | 11 (35%) | 30 (28%) |
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal