Abstract
Background & Aims
Crohn’s disease (CD) is an immunologically mediated inflammatory disease of the gastrointestinal tract. In theory, immune ablation followed by autologous hematopoietic stem cell transplantation (HSCT) can induce remission by reconstituting a new immune system.
Methods
We conducted a phase I HSCT study in 12 patients with severe CD. Candidates were less than 60 years old with a Crohn’s Disease Activity Index (CDAI) of 250–400 despite conventional therapy including infliximab. Peripheral blood stem cells were mobilized with cyclophosphamide and granulocyte colony-stimulating factor and CD34+ enriched. The immune ablative conditioning regimen consisted of 200mg/kg cyclophosphamide, and 90mg/kg equine antithymocyte globulin.
Results
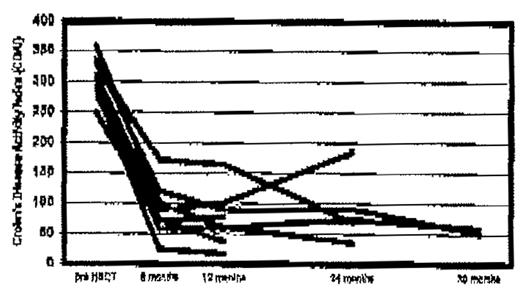
The procedure was well tolerated with anticipated cytopenias, neutropenic fever, and disease-related fever, diarrhea, anorexia, nausea, vomiting. The median days for neutrophil and platelet engraftment were 9.5 (range 8–11) and 9 (range 9–18), respectively. The infused CD34+ and CD3+ cell counts were 5.64 x 106/kg (range 1.73–9.93) and 0.59 x 104/kg (range 0.3–3.09), respectively. Initial median CDAI was 291 (range 250–358). Symptoms and CDAI improved dramatically (figure 1), and radiographic and colonoscopy findings improved gradually over months to years following HSCT. Ten out of twelve patients entered sustained remission defined by a CDAI ≤ 100. After median follow-up of 17.5 months (range 6–37), only one patient has developed recurrence of active CD which occurred 15 months post-HSCT.
Conclusion
Autologous HSCT may be peformed safely and has a marked salutary effect on CD activity. Randomized studies will be needed to confirm the efficacy of this therapy.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal