Abstract
Background: Thirty to 50% of patients with myelofibrosis with myeloid metaplasia display detectable bone marrow cytogenetic abnormalities at diagnosis with some(
Methods: The current prospective study was conducted as a follow-up of the observations from an antecedent retrospective study that identified sole abnormalities of either 13q- or 20q- as ‘favorable’ to survival (
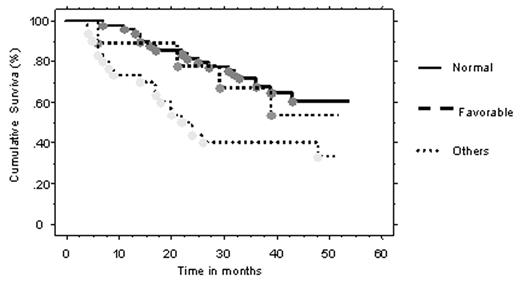
Results: Karyotypic analysis was successfully performed in a total of 88 patients (median age 61 years; 31 females) and the results were normal in 49 (56%) and abnormal in the remaining 39 patients with 9 (10%) displaying ‘favorable’, and 30 (34%) ‘other’ clonal abnormalities. At the time of study entry, 57 patients were not recieving any form of therapy, 18 were newly diagnosed, and the Dupriez prognostic score distributions were ‘0’ in 33 patients, ‘1’ in 35 and ‘2’ in 20 (
Similarly, no patient (0%) in the ‘favorable’ group transformed into acute leukemia while 6 of 30 (20%) in the ‘other’ and 5 of 49 (10%) in the normal groups did (p=0.21). In a Cox regression analysis, cytogenetic lesions other than the ‘favorable’ kind, hemoglobin below 10 g/dL, leukocytosis, hypercatabolic symptoms, increased blood blast %, blood CD 34 count above 100 x 106/L were individually associated with shortened survival. In a multivariate analysis, only hemoglobin level and leukocyte count retained their significance.
Conclusion: Single chromosomal abnormalities of either 13q- or 20q- should be considered as ‘favorable’ cytogenetic lesions in MMM while other abnormalities are associated with an adverse prognosis. The current observation explains the discrepancy in the literature regarding the prognostic relevance of cytogenetic findings in MMM and warrants additional studies to determine the value of incorporating the specific information in prognostic scoring systems.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal