Hemochromatosis is now recognized to be genetically heterogeneous and caused by mutations in at least 6 genes of iron metabolism. The majority of patients presenting symptomatically with iron overload are homozygous for a founder mutation C282Y in HFE, the gene for hereditary or type I hemochromatosis. The finding that mice homozygous for either a null allele of Hfe (Hfe–/–) or the orthologous mutation found in type I hemochromatosis (Hfe845A/845A) demonstrate elevated serum iron and develop hepatic iron overload in a pattern that recapitulates that found in humans confirms that this form of hemochromatosis does arise from loss of function of HFE. However, despite extensive studies it is still not known how mutations in HFE cause increased iron absorption and iron overload. The favored notion is that HFE together with transferrin receptor is part of an iron-sensing complex present on the basolateral surface of the intestinal crypt cells, programming the crypt cell with information about body iron requirements leading to appropriate expression of carrier molecules.1 In the case of mutated HFE, this information is faulty and leads to inappropriate absorption in relation to body iron stores. Although HFE/transferrin receptor 1 (TfR1) complexes have been detected immunologically in duodenal lysates and could theoretically modulate cellular iron uptake by influencing transferrin binding to TfR1, receptor recycling rates, or release of iron from endosomes, transfection of wild-type HFE into cultured cells has been consistently reported to induce an iron-deficient phenotype and it is difficult to reconcile the finding of iron-deficient crypt cells that demonstrate reduced uptake of transferrin iron with the presence of mutant HFE.
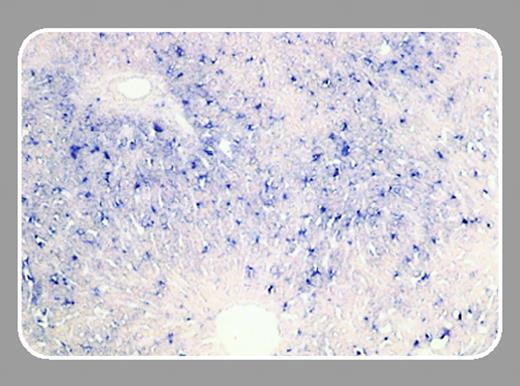
The development of a new model of HFE function has become necessary following the characterization of hepcidin, a novel peptide hormone synthesized by the liver hepatocytes that appears to have a determining effect on iron absorption and iron metabolism and provides a link with inflammation and body iron stores.2 A primary defect in hepcidin has been shown to cause iron overload in humans and in mouse models. In addition hepatic hepcidin gene expression has been found to be reduced in HFE-related hemochromatosis and Hfe- deficient mice. These findings suggest that the regulatory mechanism by which hepcidin expression is augmented in response to iron overload is HFE dependent. Hepcidin is synthesized exclusively by hepatocytes and the findings reported in this issue of Blood by Zhang and colleagues (page 1509) that Hfe mRNA and protein is predominantly expressed in liver hepatocytes not only supports the idea of linkage between 2 proteins on a regulatory pathway but also suggests that the liver and not the intestine has the central role in the pathogenesis of hemochromatosis. We suggest that there is a regulatory, iron-sensing pathway centered on the hepatocyte in which hepcidin lies downstream of HFE. The mechanism by which hepcidin expression is altered in response to iron overload is HFE dependent. Hepcidin however can also be augmented by hypoxia, erythropoiesis, and inflammation via HFE-independent pathway. Recent demonstration that hypoxia increases intestinal iron uptake independent of HFE supports this notion.3

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal