Abstract
Bivalirudin is a synthetic antithrombin sharing a sequence of 11 amino acids with the recombinant hirudin lepirudin. We investigated whether antilepirudin antibodies recognize epitopes on bivalirudin. Antilepirudin antibody–positive sera of 43 patients, treated with lepirudin for heparin-induced thrombocytopenia, were analyzed. Lepirudin- and bivalirudin-coated microtiter plates were used for antibody testing in an enzyme-linked immunosorbent assay (ELISA) system. Of the 43 sera-containing antibodies binding to lepirudin, 22 (51.2%) contained antibodies that also recognized bivalirudin. Binding of these antibodies to bivalirudin was inhibited by more than 70% by preincubation with high doses of bivalirudin. However, if lepirudin-coated microtiter plates were used, high concentrations of bivalirudin inhibited only 2 of the 43 positive sera by more than 30%. Therefore antihirudin antibodies must be polyspecific. The clinical consequences of this cross-reactivity are unknown but bivalirudin, targeted by antibodies of patients treated with lepirudin previously, could potentially boost antibody titers in such patients or even trigger an immune response by itself. Clinically significant antibody formation in response to bivalirudin monotherapy has not been observed, however. Yet, as lepirudin and antilepirudin antibodies have recently been implicated in severe anaphylactic reactions, caution is warranted when using bivalirudin in patients previously treated with lepirudin.
Introduction
Bivalirudin is a small (molecular weight [MW] 2180 Da) synthetic peptide modeled after hirudin and consists of 20 amino acids, containing 2 binding domains that bind directly and reversibly to the catalytic site and to the anion-binding exosite of thrombin.1,2 Bivalirudin is approved for use as an anticoagulant in patients with unstable angina undergoing percutaneous coronary interventions3,4 and is under investigation in patients with acute coronary syndromes,5-7 acute myocardial infarction,8-11 and cardiac surgery patients with heparin-induced thrombocytopenia (HIT). Bivalirudin has been successfully used as an alternative anticoagulant to treat patients with HIT.12,13
Hirudins are proteins 65 amino acids in length and of nonhuman origin (medical leech). Antihirudin antibody formation in patients treated with recombinant hirudins has been demonstrated in several studies. In a prospective trial, 87 (44%) of 198 HIT patients treated with lepirudin in therapeutic dose developed antihirudin antibodies of the immunoglobulin G (IgG) class.14 In another study 74% of HIT patients developed antihirudin antibodies of the IgG, IgA, and/or IgM class.15,16 The risk of immunization per time exposed seems to be in a similar range if desirudin, a recombinant (r)–hirudin similar to lepirudin, is given in prophylactic dose (desirudin 15 mg subcutaneously twice a day).17 Antibodies of patients treated with desirudin showed a 100% cross-reactivity to lepirudin and vice versa and therefore must recognize structures common to both hirudins with similar immunogenicity.17 Recently lepirudin has been linked to at least 9 cases of severe anaphylaxis, 4 of them with fatal outcome.18
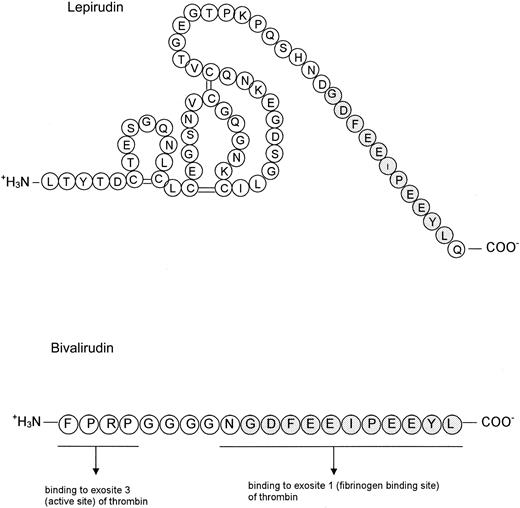
The amino acid sequence that hirudin and bivalirudin have in common binds to the exosite 1 of thrombin, as do other thrombin substrates. Clinically significant antibody formation in response to bivalirudin monotherapy seems to be low, but as immunogenicity of lepirudin is high and lepirudin and bivalirudin share a sequence of 11 amino acids (Figure 1) we sought to determine the extent of in vitro cross-reactivity of antilepirudin antibodies with bivalirudin.
Structural similarities between lepirudin and bivalirudin. The sequence of 11 amino acids in the C-terminus (gray) is identical in lepirudin (A) and in bivalirudin (B). (The 2-dimensional structure of the molecules is arbitrary.)
Structural similarities between lepirudin and bivalirudin. The sequence of 11 amino acids in the C-terminus (gray) is identical in lepirudin (A) and in bivalirudin (B). (The 2-dimensional structure of the molecules is arbitrary.)
Patients, materials, and methods
Study objective
The objective was to assess whether antilepirudin antibodies in sera of lepirudin-treated patients recognize epitopes on bivalirudin.
Sera
The study included sera from HIT patients treated with lepirudin who developed antilepirudin antibodies. Patients were treated with lepirudin in therapeutic (bolus followed by activated partial thromboplastin time [aPTT]–adjusted intravenous infusion; n = 32) or prophylactic (aPTT-adjusted intravenous infusion; n = 11) doses. Mean treatment duration was 13.9 days. All sera were stored in aliquots at –30°C, thawed, and tested. Lepirudin (Schering AG, Berlin, Germany) as well as bivalirudin (The Medicines Company, Parsippany, NJ) were obtained from the manufacturers.
Methods
An enzyme-linked immunosorbent assay (ELISA) for detection of antilepirudin IgG antibodies was performed as described before14 with the following modifications. Microtiter plate wells (high binding capacity; Greiner, Frickenhausen, Germany) were coated with either 10 μg/well lepirudin or 10 μg/well bivalirudin in coating buffer (8 mM NaH2PO4 × H2O, 53 mM Na2HPO4, pH 7.5) overnight at 18°C to 24°C; washed 4 times (0.15 m NaCl, 0.1% Tween 20, pH 7.5); incubated (60 minutes, 37°C) with sera of lepirudin antibody–positive patients (100 μL of 1:50 in sample dilution buffer [0.05 m NaH2PO4 × 1 H2O, 0.15 m NaCl, 7.5% goat serum, pH 7.5]); washed 4 times; incubated with 100 μL goat anti–human IgG–horseradish peroxidase (HRP) conjugate (Jackson, Hamburg, Germany; 60 minutes, 37°C, in sample dilution buffer); washed 4 times; and incubated with 100 μL per well substrate solution (o-phenylenediamine dihydrochloride; DAKO, Glostrup, Denmark) (30 minutes, room temperature, in the dark). The reaction was stopped by adding 100 μL 0.5 M H2SO4 and optical densities (ODs) were measured at 492 nm.
For inhibitory experiments sera were preincubated with high concentrations of either lepirudin (100 μg/mL and 400 μg/mL) or bivalirudin (1 mg/mL). As control, albumin was added in different concentrations (50, 100, 500, 1000 μg/mL).
Cutoff values were defined based on serum samples from 100 healthy blood donors. Assay results were deemed negative or positive (99% quantile of blood donor data). All samples and standards were tested in duplicate. OD values of binding experiments and of inhibitory experiments were compared by the Wilcoxon rank sum test.
Relevance of the antibodies in vivo
In 28 of 43 patients, lepirudin dose and aPTT levels during treatment were available. The aPTT courses and dose changes were analyzed.
Results
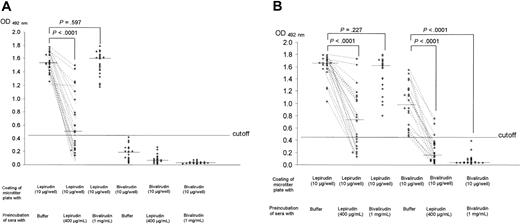
A total of 43 sera of patients who had previously developed antilepirudin antibodies were assessed. In the lepirudin-coated ELISA 43 (100%) of 43 samples gave a positive result. Twenty-one (48.8%) of 43 sera contained antibodies that recognized lepirudin but not bivalirudin. These antibodies were inhibited by preincubation with high concentrations of lepirudin (400 μg/mL) but not by high concentrations of bivalirudin (1 mg/mL; Figure 2A). Twenty-two (51.2%) of 43 sera contained antibodies that bound to lepirudin and to bivalirudin (Figure 2B). When lepirudin was coated to microtiter plates a higher OD occurred compared with bivalirudin-coated microtiter plates. Antibody binding to lepirudin was inhibited dose dependently by lepirudin in the fluid phase (mean OD with buffer, 1.600 ± 0.193; mean OD with 100 μg/mL lepirudin added, 1.191 ± 0.404; mean OD with 400 μg/mL lepirudin added, 0.739 ± 0.480), whereas high concentrations of bivalirudin (1 mg/mL) had only a minor impact on antibody binding to lepirudin (mean OD with buffer, 1.600 ± 0.193 vs mean OD with 1 mg/mL bivalirudin added, 1.487 ± 0.290; P = .227). When bivalirudin was coated, lepirudin in high concentrations inhibited antibody binding (mean OD with buffer, 0.969 ± 0.347 vs mean OD with 400 μg/mL lepirudin added, 0.231 ± 0.207; P < .0001) as did high concentrations of bivalirudin (mean OD with buffer, 0.969 ± 0.347 vs mean OD with 1 mg/mL bivalirudin added, 0.076 ± 0.085; P < .0001).
Cross-reactivity of antilepirudin antibodies with bivalirudin. Sera of 43 patients who developed antihirudin antibodies during treatment with lepirudin were incubated with lepirudin- or bivalirudin-coated microtiter plates as described under “Patients, materials, and methods.” To demonstrate binding specificity, sera were preincubated with either buffer or lepirudin in high concentrations (400 μg/mL) or bivalirudin in high concentrations (1 mg/mL), respectively. (A) Twenty-one sera contained antibodies that bound to lepirudin (lane 1) but not to bivalirudin (lane 4). Binding to lepirudin was strongly inhibited by high concentrations of lepirudin (lane 2) but only very weakly by high concentrations of bivalirudin (lane 3). Only 2 sera contained antibodies whose binding to lepirudin was inhibited by more than 30% by high concentrations of bivalirudin. (B) Twenty-two of 43 sera contained antibodies that bound to lepirudin (lane 1) and to bivalirudin (lane 4). When lepirudin was coated to microtiter plates, a higher OD occurred compared with bivalirudin-coated microtiter plates. Antibody binding to lepirudin was inhibited by high concentrations of lepirudin (lane 2), whereas high concentrations of bivalirudin had only a minor impact on antibody binding to lepirudin (lane 3). Conversely, when bivalirudin was coated, lepirudin in high concentrations inhibited antibody binding (lane 5) to a similar extent as did high concentrations of bivalirudin (lane 6).
Cross-reactivity of antilepirudin antibodies with bivalirudin. Sera of 43 patients who developed antihirudin antibodies during treatment with lepirudin were incubated with lepirudin- or bivalirudin-coated microtiter plates as described under “Patients, materials, and methods.” To demonstrate binding specificity, sera were preincubated with either buffer or lepirudin in high concentrations (400 μg/mL) or bivalirudin in high concentrations (1 mg/mL), respectively. (A) Twenty-one sera contained antibodies that bound to lepirudin (lane 1) but not to bivalirudin (lane 4). Binding to lepirudin was strongly inhibited by high concentrations of lepirudin (lane 2) but only very weakly by high concentrations of bivalirudin (lane 3). Only 2 sera contained antibodies whose binding to lepirudin was inhibited by more than 30% by high concentrations of bivalirudin. (B) Twenty-two of 43 sera contained antibodies that bound to lepirudin (lane 1) and to bivalirudin (lane 4). When lepirudin was coated to microtiter plates, a higher OD occurred compared with bivalirudin-coated microtiter plates. Antibody binding to lepirudin was inhibited by high concentrations of lepirudin (lane 2), whereas high concentrations of bivalirudin had only a minor impact on antibody binding to lepirudin (lane 3). Conversely, when bivalirudin was coated, lepirudin in high concentrations inhibited antibody binding (lane 5) to a similar extent as did high concentrations of bivalirudin (lane 6).
Albumin did not cause inhibition at any concentration tested (mean OD at 50 μg/mL, 1.654 ± 0.119; 100 μg/mL, 1.663 ± 0.124; 500 μg/mL, 1.676 ± 0.136; 1000 μg/mL, 1.502 ± 0.141; buffer instead of albumin, 1.600 ± 0.193). Each concentration was tested with 22 sera.
Of 14 evaluable patients with antibodies only reacting with lepirudin, in 8 there was a potentially enhancing effect of the antibodies (ie, aPTT increased from 57-80 seconds to 71-159 seconds while lepirudin dose was maintained [n = 3] or aPTT was stable or even increased while lepirudin dose was reduced up to 62% [n = 5]). In 4 patients there was no obvious effect. In 2 patients there was a potentially inhibitory effect associated with the antilepirudin antibodies (in one patient the aPTT decreased while keeping lepirudin dose stable and in the other, despite an increase in lepirudin dose, the aPTT decreased).
Of 14 evaluable patients with antibodies cross-reacting with bivalirudin, in 9 there was an enhancing effect and in 5 no biologic effect could be seen when aPTT and lepirudin dose changes were assessed.
Discussion
As bivalirudin and lepirudin have a segment of their respective amino acid sequences in common, cross-reactivity of antihirudin antibodies to this structurally similar site of bivalirudin is a plausible concept. Indeed, using sera of 43 well-characterized patients with antilepirudin antibodies, we confirmed this assumption: 22 sera (51.2%) contained antibodies binding to epitopes on bivalirudin (Figure 2B). Binding specificity was demonstrated by inhibition of more than 70% by preincubation with free bivalirudin. As binding of antibodies to lepirudin was not inhibited by high concentrations of bivalirudin, whereas binding to bivalirudin was inhibited by both high concentrations of lepirudin and high concentrations of bivalirudin, patient sera must contain polyspecific antibodies recognizing different epitopes on the lepirudin molecule, some of them shared with bivalirudin.
Generally lower antibody binding to bivalirudin compared with lepirudin was probably caused by the fact that bivalirudin does not share all of the epitopes to which the polyspecific response to lepirudin is directed. Thus, not all antihirudin antibodies in a particular patient serum can actually bind bivalirudin. Steric inhibition occurring after binding of the small bivalirudin molecule to the microtiter plate and different coating characteristics may also decrease antibody binding.
Antihirudin antibody formation has been demonstrated in animal experiments19,20 but only very rarely in healthy volunteers21 or in patients with acute coronary syndromes treated with hirudins.22,23 Recently it became obvious that in patients treated with lepirudin for periods of more than 5 days (eg, for treatment of heparin-induced thrombocytopenia), development of antihirudin antibodies is relatively common. These antibodies can be biologically relevant. As we observed previously14 and in this study, the most common effect of the antilepirudin antibodies was enhancement of the anticoagulatory effect (17/28; 61%), whereas inhibitory effects were much less frequent (2/28; 7%).
Two patients with allergic reactions following re-exposure to the hirudins desirudin and lepirudin have been reported.24,25 One of them was a volunteer who had received desirudin 5 years earlier and who developed urticaria after he was re-exposed twice within a 1-week interval between the subcutaneous injections.24 The second patient developed symptoms of an allergic response during re-exposure to lepirudin. Both patients tested positive for antihirudin antibodies.25
Recently lepirudin has been linked to at least 9 cases of severe anaphylaxis, 4 of them with fatal outcome. Most of the anaphylactic reactions occurred during re-exposure and in cardiac patients.18
In contrast, no clinically relevant antibivalirudin antibody formation from any study including studies in which bivalirudin was given intravenously for at least 5 days has been reported to date. Among 494 patients who received bivalirudin in clinical trials and were tested for antibodies, only 2 had positive bivalirudin antibody tests. Neither patient demonstrated clinical evidence of allergic or anaphylactic reactions.26 In a study of 222 patients27 who received bivalirudin by subcutaneous administration 2 to 3 times daily for up to 14 days, no antibody formation occurred up to 6 weeks (Dr A. G. Teuber, personal oral communication, The Medicines Company, February 2003).
Our experiments lead to 3 important implications. First, in patients who have developed antilepirudin antibodies, subsequent treatment with bivalirudin should be monitored carefully because pharmacokinetic alterations might occur by reduced renal filtration of the bivalirudin antibody complexes. As the shared structure of both molecules is the functional part, cross-reacting antihirudin antibodies should preferably bind to these epitopes, potentially exerting additional functional effects, although we did not see a major difference in the biologic effects between antibodies recognizing lepirudin alone and antibodies recognizing lepirudin and bivalirudin. Second, on a more speculative note, bivalirudin, sharing epitopes with lepirudin, might lead to boosting of antihirudin antibody titers or even formation of antibivalirudin antibodies independent of any lepirudin treatment. Third, and most important, anaphylaxis occurring in patients re-exposed to lepirudin, presumably due to antilepirudin antibodies, might also occur upon exposing such patients to bivalirudin and vice versa.
It is quite possible that the epitope generating the cross-reacting antibody may be different from those responsible for the severe immune responses upon re-exposure, given the multiple epitopes on lepirudin that trigger antibody formation and the relatively small homologous sequence between lepirudin and bivalirudin. However, for safety reasons caution is warranted when bivalirudin is used in patients who have been treated with lepirudin or desirudin.
Prepublished online as Blood First Edition Paper, September 25, 2003; DOI 10.1182/blood-2003-07-2229.
Supported by Deutsche Forschungsgemeinschaft Gr 1096/2-4 and by the German Federal Ministry for Education and Research (NBL3 program, reference 01 ZZ0103).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal