CLINICAL OBSERVATIONS, INTERVENTIONS, AND THERAPEUTIC TRIALS
Twenty-three years ago, Green and Lechner1 published the first survey of patients with spontaneous development of factor VIII inhibitors. That paper explored the epidemiology and other clinical characteristics in 215 patients with this rare disorder. Sixteen years ago, Lottenberg, Kentro, and I2 wrote an article addressing the natural history of factor VIII inhibitors, illustrating that not much was certain regarding treatment of this disorder. We also pointed out that spontaneous remission may occur in up to a third of the patients, yet sometimes taking many months to occur. We also confirmed that even in patients with no detectable factor VIII activity, hemarthroses were unusual, whereas soft tissue hemorrhage was characteristic. When one receives a telephone call consultation (almost invariably on a Friday afternoon) from a referring hematologist concerning an elderly patient who had never before experienced abnormal hemostasis yet is now bruising and has a prolonged partial thromboplastin time (PTT), the diagnosis is almost certain, despite the fact that this disease occurs in approximately only one in a million people.FIG1
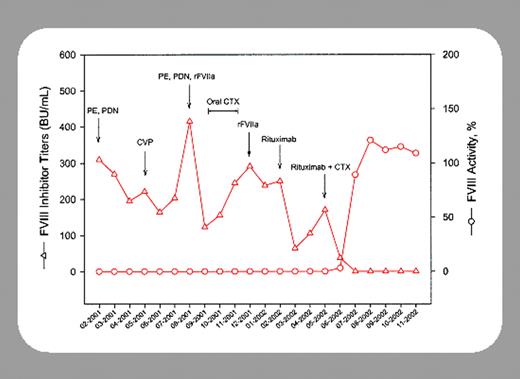
In this issue, Stasi and colleagues (page 4424) describe successful treatment of acquired hemophiliacs with rituximab. Their paper adds to the experience from the initial single patient described by Kain and colleagues3 as well as the 4 patients described by Wiestner and colleagues.4 Stasi's group reported 10 more cases. Although these 3 reports combined represent only 15 cases (hardly the size of mega-cardiology studies), the stereotypic pattern of response enhances the likelihood that these observations are valid.
The reader of these 3 reports is quite taken by the suddenness and durability of response in patients who had heretofore failed numerous other treatments, during which time the protraction of this autoimmune disorder would argue that these cases were not just transient. The response seems superior to that of the litany of other treatments tried in the past, such as other methods of immunosuppression to include glucocorticosteriods, cyclophosphamide, and others. As such, acquired factor VIII inhibitors giving rise to acquired hemophilia may be added to the list of other autoimmune hematologic disorders for which treatment using this agent shows promise, including idiopathic thrombocytopenic purpura (ITP) and autoimmune hemolytic anemia. Of interest, Stasi and colleagues also report that 3 of their patients had concomitant lupus anticoagulant activity as well as anti-factor VIII; both seemed to respond.
Rituximab administration appeared to be safe. While patients experienced severe depletion of CD19+ cells (although the total number of patients treated is small), it is interesting that no infectious sequelae were noted.
We have traditionally regarded 2 treatment phases for this rare disease: namely, an acute treatment to increase hemostasis with agents such as factor eight inhibitor bypassing activity (FEIBA), porcine factor VIII, or activated factor VIIa, and, secondly, immunomodulation to decrease anti-factor VIII production for long-term maintenance. Treatment appeared to work so rapidly in the majority of Stasi et al's patients that one might consider such therapy reasonable to initiate at the time of diagnosis for both the acute and chronic phases. Should such therapy be considered “first line” in such patients? This is not clear and Stasi and colleagues do not claim that it should be. However, when pressed with the clinical needs of a hemorrhaging patient and the extreme costs and considerable side effects of some alternative agents, it seems appropriate to consider rituximab as initial therapy because 8 of the 10 patients studied responded within a few weeks.
Although one is tempted to state “further studies are needed to verify these observations,” the fact remains that this is a rare and dangerous disease and it is likely that, without a coordinated effort (which is still possible), there will not be any randomized controlled trials.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal