CLINICAL OBSERVATIONS, INTERVENTIONS, AND THERAPEUTIC TRIALS
It was proposed more than 25 years ago that atherosclerosis arises as a response of the vascular wall to endothelial injury. Evidence accumulated in the last decade showed that this injury could be due to endothelial apoptosis. Most known risk factors for atherosclerosis induce, while treatments and prophylactic interventions have the potential to decrease, endothelial apoptosis.1 Many of the findings associated with atherosclerosis, such as endothelial dysfunction and activation, can be caused by endothelial apoptosis, and apoptotic endothelial cells are found on the surface of atherosclerotic plaques.1-3
Young and predominantly female patients with systemic lupus erythematosus (SLE) are an unusual group manifesting an extraordinarily strong predisposition for the development of early-onset and accelerated atherosclerosis. In addition to the usual risk factors, SLE itself predisposes to premature atherosclerosis in a manner that does not always correlate with markers of systemic inflammation or measures of disease activity.4
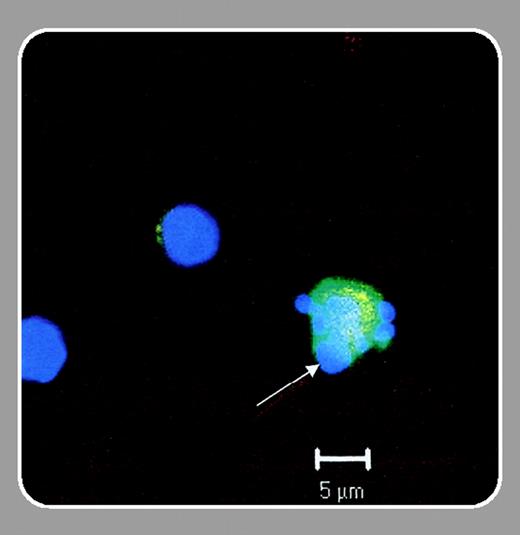
What causes premature and accelerated atherosclerosis in patients with SLE? In this issue of Blood, Rajagopalan and colleagues (page 3677) describe increased numbers of apoptotic endothelial cells in the peripheral blood of patients with SLE. They compare patients with SLE to 2 control groups: healthy subjects without presence of usual risk factors for atherosclerosis, and patients with known coronary artery disease (CAD). The markedly higher numbers of apoptotic endothelial cells found in young women with SLE, when compared with the older group of predominantly male patients with CAD, suggest that endothelial apoptosis may be responsible for premature and accelerated atherosclerosis in patients with SLE. The authors fail to detect significant differences in the unequal numbers of circulating apoptotic endothelial cells between the 2 control groups in this study, which could be due to the relatively stable clinical status and the use of endothelial antiapoptotic treatments1 (statins, aspirin, β-blockers, angiotensin-converting enzyme [ACE] inhibitors) in the CAD group. They do, however, find for the first time in human subjects a significant correlation between numbers of apoptotic endothelial cells and endothelial dysfunction; in a previously described primate model, endothelial dysfunction occurred after endothelial cell loss from the vascular wall and was due to endothelial apoptosis.2
The results of the study by Rajagopalan et al suggest that future investigations should focus on specific endothelial proapoptotic and antiapoptotic factors that may be relevant in patients with SLE. These include the known proapoptotic (antiendothelial cell antibodies, anti-dsDNA antibodies, lupus anticoagulant, inflammatory mediators, neutrophil proteases) and antiapoptotic (glucocorticoids, cyclosporine A) agents.1,5 One approach could involve exposure of endothelial cells in vitro to serum from patients with SLE, neutralization of known proapoptotic factors to gain an impression of their relative importance in SLE, and testing of available antiapoptotic stimuli as agents that may be useful for subsequent clinical trials. This may permit a rational advance toward therapies that will improve the prognosis in patients with SLE.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal