We report a case of cutaneous Epstein Barr Virus (EBV)-positive B-cell lymphoproliferative disease in a 70-year-old female, who was treated with 500 mg/d imatinib mesylate (Gleevec; Novartis, Zurich, Switzerland) for chronic myeloid leukemia (CML).
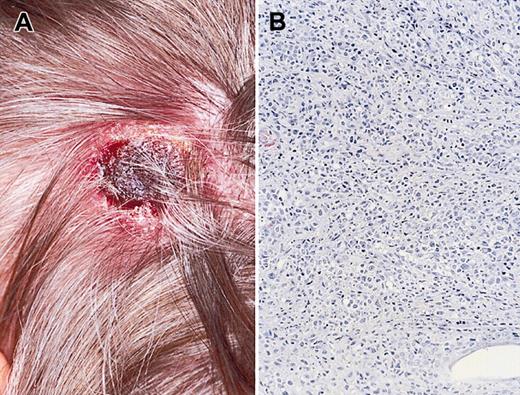
The woman had previously been treated with 1000 mg hydroxyurea twice daily, resulting in stable disease. However, upon development of a leg ulcer, hydroxyurea was discontinued and ambulant compression therapy in combination with 2 × 200 mg/d pentoxyfilline (PTX) and 100 mg/d ascal was initiated. Her CML progressed, and 500 mg/d imatinib mesylate was started. Subsequently, her leukocyte count decreased from 9.9 × 109/L before treatment to 1.3 × 109/L after 2 months of treatment. Shortly after starting imatinib mesylate she noticed a rapidly growing, ulcerating tumor on her head (Figure 1A). A biopsy showed a diffuse proliferation of large, atypical, immunoblastic B cells (Figure 1B) that strongly expressed CD79a and CD30 and were monotypic immunoglobulin G (IgG) lambda-positive. Most large atypical cells stained positive for EBV-encoded RNA 1 (EBER-1), mRNAs, and latent membrane protein 1 (LMP-1) and EBV nuclear antigen 1 (EBNA1) proteins, whereas focal expression was found for BamHI fragment Z left frame 1 (BZLF1). There was no expression for EBV early antigen (EA), EBV viral capsid antigen (VCA), and membrane antigen (MA). RNA in situ hybridization showed expression of EBER-1 and EBER-2. EBV serology (enzyme-linked immunosorbent assay [ELISA]; Biotest, Dreieich, Germany) demonstrated IgG, against EBV-VCA, EBV-NA (nuclear antigen), and EBV-EA. After spontaneous resolution of the tumor, the IgG EBV-EA levels gradually lowered, but IgG VCA and NA remained stable. An immunoblot assay and synthetic peptide ELISA test demonstrated a strong IgG response against VCA (p18 en p40) and the lytic switch protein Zebra. There was a high IgA response against VCA (P18), without significant reactivity to other EBV antigens. Combined, these findings are consistent with EBV-related lymphoproliferation due to EBV reactivation and persistent EBV replication.
Clinical presentation and histologic section of the skin tumor stained with hematoxilin and eosin showing diffuse proliferation of large atypical blasts. Clinical (A) and histologic (B) presentation of primary cutaneous EBV+ lymphoproliferative disease. Original magnification, × 200 (B).
Clinical presentation and histologic section of the skin tumor stained with hematoxilin and eosin showing diffuse proliferation of large atypical blasts. Clinical (A) and histologic (B) presentation of primary cutaneous EBV+ lymphoproliferative disease. Original magnification, × 200 (B).
Staging procedures were negative and diagnosis of primary cutaneous EBV-related B-cell lymphoproliferation was made, and the dose of the imatinib mesylate was lowered to 400 mg/d. This resulted in a rise in the patient's leukocyte count to 2.8 × 109/L and spontaneous resolution of the tumor.
EBV-associated lymphoid proliferations are a heterogeneous group of lymphoproliferative diseases occurring in the setting of immunosuppression in which the level of T-cell depletion is considered to be one of the most important risk factors.1
Primary cutaneous EBV-associated B-cell lymphoproliferative disease generally has a good prognosis, and after recovery of the immunocompromised status a spontaneous remission often is observed.2 The spontaneous remission of the tumor after restoration of the leukocyte count in the presented patient is in line with these observations.
In addition to imatinib mesylate, the potential role of PTX deserves mentioning. In vitro and in vivo studies demonstrated that PTX may promote replication of human cytomegalovirus (CMV) by activation of the CMV immediate early promoter. Because this activation is mediated in a nonspecific way, PTX may have affected replication of EBV in this patient in a similar manner.3
Early recognition of EBV-related posttransplantation lymphoproliferative disease is crucial, because in these early phases restoration of immunosuppression may still result in disappearance of the lesions. In later stages, when a frank lymphoma develops, treatment is more difficult and the prognosis is not as good.
We would like to thank Anneke Brand (Department of Hematology, Leiden University Medical Center [LUMC]) and Louis C. M. Kroes (Department of Microbiology and Virology, LUMC) for clinical advice and valuable comments.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal