Plasmacytoid dendritic cells (pDCs) contribute to innate antiviral immune responses by producing type I interferons (IFNs) upon exposure to enveloped viruses. However, their role in adaptive immune responses, such as the initiation of antiviral T-cell responses, is not known. In this study, we examined interactions between blood pDCs and influenza virus with special attention to the capacity of pDCs to activate influenza-specific T cells. pDCs were compared with CD11c+ DCs, the most potent antigen-presenting cells (APCs), for their capacity to activate T-cell responses. We found that like CD11c+ DCs, pDCs mature following exposure to influenza virus, express CCR7, and produce proinflammatory chemokines, but differ in that they produce type I IFN and are resistant to the cytopathic effect of the infection. After influenza virus exposure, both DC types exhibited an equivalent efficiency to expand anti–influenza virus cytotoxic T lymphocytes (CTLs) and T helper 1 (TH1) CD4+ T cells. Our results pinpoint a new role of pDCs in the induction of antiviral T-cell responses and suggest that these DCs play a prominent role in the adaptive immune response against viruses.
Introduction
There are 2 main dendritic cell (DC) subsets that have been identified in humans: the CD11c+myeloid DCs, which include Langherans cells and dermal and interstitial DCs, and the CD11c−/CD123+/CD4+plasmacytoid DCs (pDCs).1 During viral infection, CD11c+ DCs play an important role in adaptive antiviral immune responses by acquiring and processing viral antigens into peptides for major histocompatibility complex (MHC) presentation to T cells in secondary lymphoid organs.2pDCs, also known as type I interferon (IFN)–producing cells (IPCs) and previously referred to as plasmacytoid lymphocytes or plasmacytoid monocytes, are located in blood and in secondary lymphoid organs.3 They express CD4, CD123 (IL-3R chain α), and high levels of HLA-DR molecules, but lack expression of CD11c and other myeloid-related markers (eg, CD11b, CD13, and CD33). pDCs participate in innate antiviral responses by producing large numbers of type I IFNs (-α, -β, and -ω) when exposed to different types of viruses (influenza virus, herpes simplex virus [HSV], and HIV).4-7
The involvement of pDCs in the adaptive antiviral immune responses, especially antiviral T-cell responses, has not been demonstrated. For instance, pDCs' ability to acquire, process, and present viral antigens to T cells after virus exposure has not yet been addressed. However, several observations suggest that pDCs, after being in contact with virus, may play a role in the initiation of antiviral T-cell responses. Indeed, immature pDCs are poor T-cell stimulators, whereas pDCs matured by HSV or influenza virus expand allogeneic naive T cells as efficiently as mature CD11c+ DCs.7,8 pDCs exposed either to CD40L or to influenza virus express CCR7 and migrate in response to CCL19, a chemokine produced in the T-cell area of lymph nodes.9,10 Furthermore, pDCs are found in increased number in secondary lymphoid organs during inflammation.11
In this study, we investigated the effects of influenza virus exposure on blood-purified pDCs in vitro and the capacity of these cells to acquire and present viral antigens to CD8+ and CD4+ T cells. We found that, unlike CD11c+ DCs, pDCs are resistant to influenza virus infection, characterized by reduced virus-induced apoptosis and influenza protein expression. However both types of DCs have an equivalent ability to induce the proliferation and the differentiation of anti-influenza CTLs and T helper 1 (TH1) CD4+ T cells. Therefore, pDCs likely play an important role in the initiation of antiviral T-cell responses via several mechanisms: through production of IFN-α, which initiates viral resistance, maintains pDC viability, and promotes antiviral T-cell responses; and via direct activation of CD4+ and CD8+ T cells following processing of influenza antigens.
Materials and methods
T cells, pDCs, and CD11c+ DC purifications
Leukocyte-enriched buffy coats were obtained from the New York Blood Center (New York, NY). Peripheral blood mononuclear cells (PBMCs) were separated by density gradient centrifugation on Ficoll-Hypaque (Amersham Pharmacia Biotech, Piscataway, NJ). HLA-A*0201+ and HLA-DR*0401+ PBMCs were identified by immunofluorescence using monoclonal antibodies (mAbs) against HLA-A2 (HB82; American Type Culture Collection [ATCC], Manassas, VA) and HLA-DR4 (Accurate Chemical & Scientific), respectively. T cells were enriched from PBMCs by magnetic-bead (M450, Dynal, Oslo, Norway) depletion of monocytes, B cells, natural killer (NK) cells, and erythrocytes using mAbs against CD14, CD19, CD56, and glycophorin-A. pDCs and CD11c+ DCs were initially enriched from PBMCs by magnetic-bead depletion of T and B lymphocytes, monocytes, NK cells, and erythrocytes using mAbs against CD3, CD19, CD14, CD56, and glycophorin A. pDCs (CD3−, CD11c−, CD14−, CD16−, CD20−, and CD4+ cells) and CD11c+DCs (CD3−, CD11c+ high, CD14−, CD16−, CD20−, and CD4−/+ cells) were then purified from the enriched population by fluorescence-activated cell sorting (FACSVantage; Becton Dickinson [BD], Franklin Lakes, NJ) using fluorescein isothiocyanate (FITC)–conjugated mAbs against CD3, CD14, CD16, and CD20 (BD); phycoerythrin (PE)–conjugated mAb against CD11c (BD); and PE–cytochrome 5 (cy5)–conjugated mAb against CD4 (Caltag, Burlingame, CA). pDCs and CD11c+ DCs were more than 99% pure.
pDC and CD11C+ DC culture
Portions of obtained DCs (Flu pDCs and Flu CD11c+DCs) were cultured with 1000, 400, and 100 hemagglutinin unit (HAU)/mL live influenza A virus strain Aichi/68 (SPAFAS, Wilmington, MA) in RPMI 1640 medium with 20 μg/mL gentamicin (Gibco BRL, Grand Island, NY) and 1 mM HEPES (N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid; Mediatech, Kansas City, MO). In some experiments, they were also cultured with 1000 HAU/mL influenza virus previously boiled or heat inactivated at 56°C for 30 minutes. After one hour, pooled human serum (PHS) was added to cultures to block further infection (5% volume). Other portions of DCs (IL-3 pDCs and CD11c+ DCs) were cultured in RPMI 1640 medium containing 5% PHS and, for pDCs, 20 ng/mL IL-3 (R&D, Minneapolis, MN). DCs were cultured in 96-well flat-bottom plates at 106 cells/mL. After 16 hours, supernatants were collected and tested by enzyme-linked immunosorbent assay (ELISA) for the presence of IFN-α (Endogen, Rockford, IL), CXCL8, CXCL10, CCL3, and CCL5 (R&D). DCs were harvested, washed, and counted for viable cells. For T-cell/DC coculture experiments, IL-3 pDCs and CD11c+ DCs (HLA-A*0201+ or HLA-DR*0401+) were pulsed with peptides (influenza MP(58-66) GILGFVFTL or influenza HA(307-319) PKYVKQNTLKLAT) for 1 hour at 4°C and washed.
Phenotype
DCs were stained with FITC-conjugated mAbs against HLA-DR (Iotest, Beckman Coulter, Miami, FL), CD83 (Pharmingen, Franklin Lakes, NJ), CD86 (Pharmingen), PE-conjugated mAb against CD123 (Pharmingen), or the respective FITC- or PE-conjugated isotype control mAbs (Pharmingen). For CCR7 expression, pDCs were stained with mAb against CCR7 (Pharmingen) followed by a biotin anti–mouse IgM (Pharmingen) and then PE-conjugated streptavidin (Pharmingen). For influenza matrix protein (MP) intracellular staining, DCs were fixed with phosphate-buffered saline (PBS) containing 4% paraformaldehyde and stained with a mAb against influenza MP protein (HB64; ATCC) and an FITC-conjugated goat antimouse mAb (Biosource, Camarillo, CA) in the presence of 0.1% saponin. Fluorescence was analyzed by flow cytometry on a FACScan using Cell Quest Software (BD).
CCL19 migration assay
IL-3 pDCs or influenza virus–infected pDCs (5 × 104) were incubated in 100 μL RPMI containing 5% PHS in the upper chamber of a transwell 24-well plate with 5.0-μM pore size (Corning, Somerset, NJ). The lower chamber contained 500μL of RPMI containing 5% PHS with or without 25 ng/mL CCL19 chemokine (R&D). After 2 hours, cells in the lower chamber were harvested and counted.
DC/T-cell clone coculture
Flu16, an HLA-A*0201–restricted MP(58-66)-specific CD8+ T-cell clone, and HA136, a DRα1*0101/DRβ*0401-restricted influenza HA(307-319)–specific CD4+ T-cell clone, were isolated and cultured as previously described.12Then, 105 Flu pDCs, Flu CD11c+ DCs, peptide-pulsed IL-3 pDCs, and CD11c+ DCs were cocultured with or without 105 Flu16 or HA136 T-cell clone, in a 96-well U-bottom plate in 200 μL RPMI and 5% PHS. After 24 hours, 50 μL supernatants was collected and tested for IFN-γ by ELISA (Pharmingen). After 3 days, 4 μCi/well (0.148 MBq)3H-thymidine was added for 12 hours. Cells were then harvested to assess proliferation.
Expansion of HLA-A*0201–restricted influenza MP(58-66)-specific memory CTLs
Flu pDCs, Flu CD11c+ DCs, 1 μM MP peptide-pulsed IL-3 pDCs, or CD11c+ DCs (2 × 104) were cocultured with 2 × 105autologous T cells in 96-well U-bottom plate in 200 μL Yssel medium (Gemini Bio-Products, Woodland, CA) containing 20 μg/mL gentamicin, 1 mM HEPES, and 5% PHS. Then, 7 days later, part of the T cells were washed and stained with a PE-conjugated tetramer of MP(58-66)/HLA-A*0201 or LMP2/HLA-A*0201 complexes and an FITC-conjugated CD8 mAb (BD). Fluorescence was analyzed by flow cytometry. The other portion was restimulated by T2 cells pulsed with or without 10 μM MP peptide in IFN-γ, IL-4, and IL-10 enzyme-linked immunospot (ELISPOT) assays to measure the expansion of MP-specific CTLs as previously described.13 In some experiments, cytolytic activity of these T-cell populations was assessed by a standard chromium 51 (51Cr) release assay using T2 cells as target cells, as previously described.13
Expansion of influenza A virus–specific memory CD4 T cells
Flu pDCs or Flu CD11c+ DCs (2 × 104) were cocultured with 2 × 105autologous T cells in 96-well U-bottom plate in 200 μL Yssel medium (Gemini Bio-Products) containing 20 μg/mL gentamicin, 1 mM HEPES, and 5% PHS. Autologous monocytes were cultured with IL-4 and granulocyte-macrophage colony-stimulating factor (GM-CSF) for 7 days, and monocyte-conditioned medium was added at day 5 to obtain monocyte-derived matured DCs, as previously described.14Then, 7 days later, T cells were restimulated by monocytes derived from matured DCs infected or not with influenza virus in the presence of 10 μg/mL brefeldin-A (Sigma, St Louis, MO). After 6 hours, cells were stained with a PE-cy5–conjugated mAb against CD4 (Caltag) and then fixed with PBS containing 4% paraformaldehyde and stained with PE-conjugated mAbs against IFN-γ, IL-4, or IL-10 (Pharmingen) in the presence of 0.1% saponin. Fluorescence was analyzed by flow cytometry.
Results
Maturation of pDCs and CD11c+ DCs by influenza virus
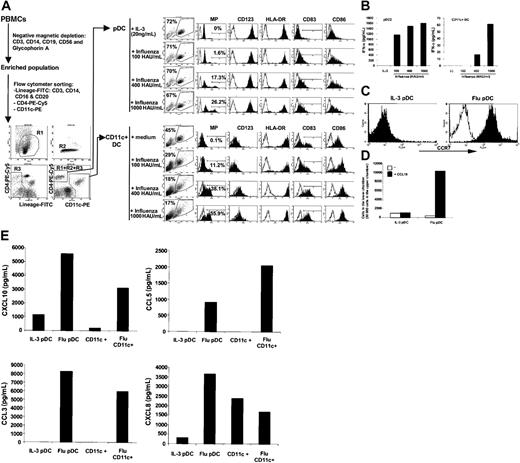
To evaluate pDC and CD11c+ DC interactions with influenza virus, DCs were purified from PBMCs by a 2-step procedure.7 DCs were first pre-enriched by magnetic bead depletion of monocytes, NK cells, erythrocytes, and B and T cells resulting in the removal of 88.7% (± 4.2%) of PBMCs. pDCs (CD3−, CD11c−, CD14−, CD16−, CD20−, and CD4+) and CD11c+ DCs (CD3−, CD11c+, CD14−, CD16−, CD20−, and CD4−/+) were then purified from the enriched population by flow cytometry sorting. Yields of pDCs and CD11c+ DCs were 0.124% (± 0.026%) and 0.216% (± 0.114%) of the starting population of PBMCs, respectively. Reanalysis of pDCs and CD11c+ DCs showed a purity of 99%. Furthermore 100% of pDCs expressed CD123 (Figure1A).
pDC and CD11c+ DC maturation by influenza virus.
pDCs and CD11c+ DCs were obtained by magnetic bead depletion and fluorescence activated cell sorting. pDCs were cultured with IL-3 or influenza virus, while CD11c+ DCs were cultured with or without influenza virus. (A) Intracellular influenza MP expression and surface CD123, HLA-DR, CD83, and CD86 expression after 16 hours of culture. (B) Detection of IFN-α in culture supernatants as measured by ELISA. (C) Surface expression of CCR7 by pDCs after 16 hours. Note the different Y-axis scale in left versus right panels. (D) Migration of pDCs toward CCL19 after 2 hours. White bars represent conditions with no CCL19 in the lower chamber; black bars, with 25 ng/mL CCL19 in the lower chamber. (E) Presence of chemokines (CXCL8, CXCL10, CCL3, and CCL5) in culture supernatants as measured by ELISA.
pDC and CD11c+ DC maturation by influenza virus.
pDCs and CD11c+ DCs were obtained by magnetic bead depletion and fluorescence activated cell sorting. pDCs were cultured with IL-3 or influenza virus, while CD11c+ DCs were cultured with or without influenza virus. (A) Intracellular influenza MP expression and surface CD123, HLA-DR, CD83, and CD86 expression after 16 hours of culture. (B) Detection of IFN-α in culture supernatants as measured by ELISA. (C) Surface expression of CCR7 by pDCs after 16 hours. Note the different Y-axis scale in left versus right panels. (D) Migration of pDCs toward CCL19 after 2 hours. White bars represent conditions with no CCL19 in the lower chamber; black bars, with 25 ng/mL CCL19 in the lower chamber. (E) Presence of chemokines (CXCL8, CXCL10, CCL3, and CCL5) in culture supernatants as measured by ELISA.
We cultured pDCs and CD11c+ DCs with different quantities of influenza virus to evaluate effects of infection. Both types of DCs underwent maturation following virus exposure as noted by increased expression of HLA-DR, CD83, and CD86 (Figure 1A). However, pDCs were resistant to the cytopathic effect of influenza virus, whereas CD11c+ DCs were sensitive, resulting in the death of the majority of the cells (see forward scatter [FSC]/side scatter [SSC] dot plot in Figure 1A). In addition, a smaller fraction of pDCs expressed influenza virus MP compared with the CD11c+ DCs. Resistance to influenza infection by pDCs is likely due to their strong production of type I IFN, such as IFN-α (Figure 1B), and to their constitutive expression of MxA, a protein with antiviral activity.8 In contrast, CD11c+DCs produced very low levels of IFN-α compared with pDCs, as described previously7,11 and shown in Figure 1B. Interestingly, we confirmed that pDCs exposed to influenza virus express CCR7, a receptor for CCL19 and CCL21, chemokines produced in the T-cell area of lymph nodes (Figure 1C and Jarrossay et al9). Furthermore, we show that this CCR7 expression by pDCs allows them to migrate toward the chemokine CCL19 (Figure 1D). Therefore, pDCs show qualitative differences from CD11c+ DCs following influenza virus exposure: resistance to the virus' cytopathic effects, sustained viral antigen expression, and production of IFN-α.
In addition to IFN-α, we also measured the production of 8 chemokines: CXCL8 (IL-8), CXCL9 (Mig), CXCL10 (IP-10), CCL3 (MIP1-a), CCL5 (RANTES), CCL7 (MCP-3), CCL8 (MCP-2), and CCL22 (MDC). We observed production of CXCL10, CCL3, and CCL5 both by the pDCs and the CD11c+ DCs in response to influenza virus (Figure 1E), with the exception of one donor where comparable amounts of these 3 chemokines were produced by pDCs cultured with IL-3 and influenza virus. pDCs also produce CXCL8 in response to the virus, whereas CD11c+ DCs express this chemokine constitutively. The production of CCL22 was highly variable from one donor to another, with consistently higher production by CD11c+ DCs cultured alone (data not shown). We failed to detect any CXCL9, CCL7, and CCL8 production by pDCs and CD11c+ DCs (data not shown). Collectively, these data suggest a similar chemokine production profile by pDCs and CD11c+ DCs.
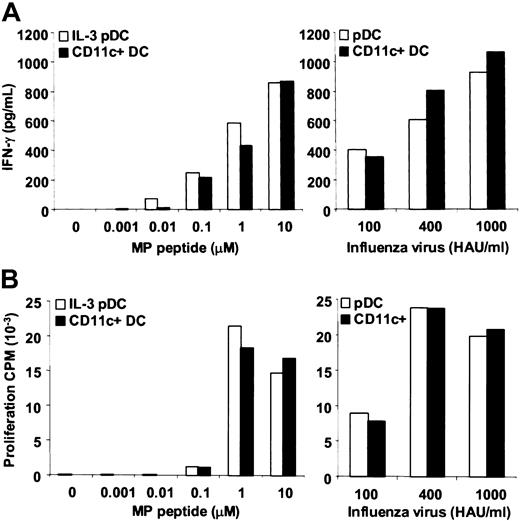
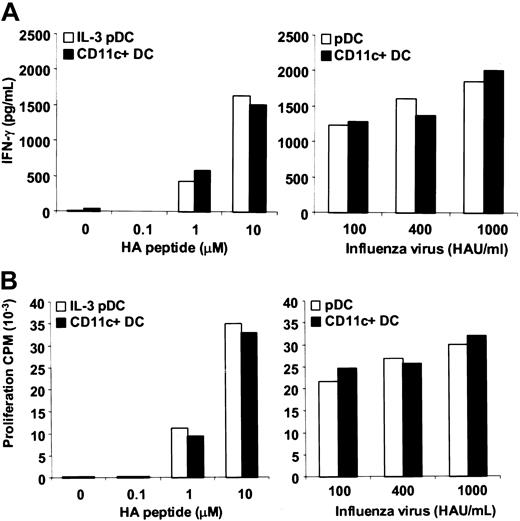
Capacity of pDCs to activate anti–influenza virus CD8+ CTLs and CD4+ T-cell clones
Mixed lymphocyte reactions (MLRs) have shown that pDCs exposed either to HSV or influenza virus are as efficient as CD11c+DCs in amplifying allogeneic T cells, supporting the idea that pDCs activated following virus encounter play an important role in activating and skewing T-cell response.7,8 15 However, pDCs have never been tested to determine whether they acquire and process viral antigens and directly activate virus-specific T-cell responses. By using Flu16, an HLA-A*0201–restricted influenza MP(58-66)–specific CD8+ CTL, clone and HA136, a DRα1*0101/DRβ*0401–restricted influenza HA(307-319)–specific CD4+ T-cell clone, we addressed whether pDCs previously exposed to influenza virus or antigens could induce antigen-specific responses. pDCs and CD11c+ DCs demonstrated the same efficiency to induce IFN-γ production and proliferation of both CD8+ and CD4+ T-cell clones, whether the viral epitopes were exogenous peptides or were derived from the processing of viral protein after influenza virus infection (Figures2-3). In several experiments, proliferation of both T-cell clones in response to influenza virus–infected DCs was as strong as or stronger than the proliferation induced by DCs pulsed with an optimal dose of peptide. This is probably due to the high degree of maturation that takes place following exposure of DCs to the virus.
Comparable efficiency of pDCs and CD11c+ DCs to stimulate an influenza MP–specific CD8+ T-cell clone.
Flu16, an HLA-A*0201–restricted influenza MP(58-66)–specific CD8+ T-cell clone, was cocultured with HLA-A*0201+ pDCs or CD11c+ DCs infected by influenza virus or pulsed with influenza MP(58-66) peptide. (A) After 24 hours, IFN-γ in the coculture supernatants was measured by ELISA. (B) After 3 days,3H-thymidine was added for 12 hours to measure proliferation. CPM indicates counts per minute.
Comparable efficiency of pDCs and CD11c+ DCs to stimulate an influenza MP–specific CD8+ T-cell clone.
Flu16, an HLA-A*0201–restricted influenza MP(58-66)–specific CD8+ T-cell clone, was cocultured with HLA-A*0201+ pDCs or CD11c+ DCs infected by influenza virus or pulsed with influenza MP(58-66) peptide. (A) After 24 hours, IFN-γ in the coculture supernatants was measured by ELISA. (B) After 3 days,3H-thymidine was added for 12 hours to measure proliferation. CPM indicates counts per minute.
Comparable efficiency of pDCs and CD11c+ DCs to stimulate an influenza HA–specific CD4+ T-cell clone.
HA136, a DRα1*0101/DRβ*0401-restricted influenza HA(307-319)–specific CD4+ T-cell clone, was cocultured with DRα1*0101/DRβ*0401+ pDCs or CD11c+ DCs infected by influenza virus or pulsed with influenza HA(307-319) peptide. (A) After 24 hours, IFN-γ in the coculture supernatants was measured by ELISA. (B) After 3 days,3H-thymidine was added for 12 hours to measure proliferation.
Comparable efficiency of pDCs and CD11c+ DCs to stimulate an influenza HA–specific CD4+ T-cell clone.
HA136, a DRα1*0101/DRβ*0401-restricted influenza HA(307-319)–specific CD4+ T-cell clone, was cocultured with DRα1*0101/DRβ*0401+ pDCs or CD11c+ DCs infected by influenza virus or pulsed with influenza HA(307-319) peptide. (A) After 24 hours, IFN-γ in the coculture supernatants was measured by ELISA. (B) After 3 days,3H-thymidine was added for 12 hours to measure proliferation.
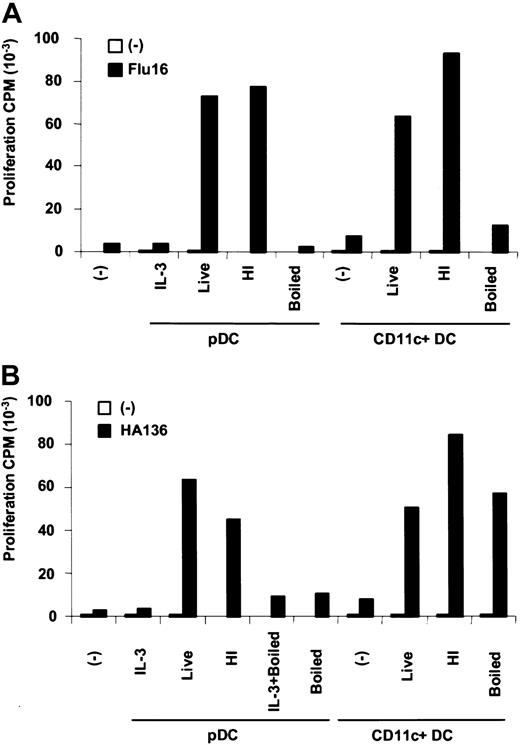
Presentation of influenza virus antigens by pDCs and CD11c+ DCs from a different source of antigens
We showed previously that CD11c+ DCs can present influenza-derived antigens from live and nonreplicating influenza virus with equal efficiency.13,16 The nonreplicating virus (heat inactivated at 56°C or ultraviolet irradiated) retains fusogenic capacity allowing entry of the capsid from endosome to cytoplasm, which is then processed and presented to both CD4+ and CD8+ T cells. We compared pDCs and CD11c+ DCs in their capacity to present different sources of influenza antigens: live influenza virus, able to infect and initiate viral protein expression in DCs (Figure 1A); heat inactivated (HI) influenza virus, able to infect DCs, but unable to initiate viral protein synthesis (data not shown); and boiled influenza virus, unable to infect DCs since it has lost its fusogenic capacity. Antigens from boiled influenza virus, however, can be processed by CD11c+DCs within endosomes to be presented to CD4+ T cells.16
Both DC subsets exposed to live or HI influenza viruses demonstrated a comparable efficiency to present influenza antigens to the CD4+ and the CD8+ T-cell clones (Figure4). This result suggests that extensive new influenza virus protein expression is not required within either DC subset and that viral particles entering the DCs are a sufficient source of antigen for processing and presentation to T cells.
Influence of antigen forms on influenza antigen HLA class I and II presentation by pDCs and CD11c+ DCs.
(A) Flu16, an HLA-A*0201–restricted influenza MP(58-66)-specific CD8+ T-cell clone, was cocultured with HLA-A*0201+ pDCs or CD11c+ DCs previously exposed to live, heat-inactivated (HI) or boiled influenza virus. After 3 days, 3H-thymidine was added for 12 hours to measure proliferation. (B) HA136, a DRα1*0101/DRβ*0401-restricted influenza HA(307-319)–specific CD4+ T-cell clone, was cocultured with DRα1*0101/DRβ*0401+ pDCs or CD11c+ DCs previously exposed to live, heat-inactivated or boiled influenza virus. After 3 days,3H-thymidine was added for 12 hours to measure proliferation.
Influence of antigen forms on influenza antigen HLA class I and II presentation by pDCs and CD11c+ DCs.
(A) Flu16, an HLA-A*0201–restricted influenza MP(58-66)-specific CD8+ T-cell clone, was cocultured with HLA-A*0201+ pDCs or CD11c+ DCs previously exposed to live, heat-inactivated (HI) or boiled influenza virus. After 3 days, 3H-thymidine was added for 12 hours to measure proliferation. (B) HA136, a DRα1*0101/DRβ*0401-restricted influenza HA(307-319)–specific CD4+ T-cell clone, was cocultured with DRα1*0101/DRβ*0401+ pDCs or CD11c+ DCs previously exposed to live, heat-inactivated or boiled influenza virus. After 3 days,3H-thymidine was added for 12 hours to measure proliferation.
When exposed to boiled influenza virus, both DC subsets were unable to present viral antigen to the CD8+ T-cell clone (Figure 4A), consistent with our earlier finding that boiling disrupts the virus' fusogenic capacity, hence entry into the cytoplasm. However, in the same experiment, only the CD11c+ DCs, but not the pDCs, were able to activate the CD4+ T-cell clone (Figure 4B). The absence of viral antigen presentation from boiled influenza virus by pDCs to the CD4+ T-cell clone was first attributed to the fact that the boiled virus failed to activate IFN-α production by the pDCs (data not shown), affecting their survival during the 16-hour in vitro culture (10%-20% live pDCs recovered). This same experiment was then repeated with addition of IL-3 to maintain pDC survival (60%-80% live pDCs recovered). In this condition, pDCs were still unable to present viral antigen to the CD4+ T-cell clone (Figure 4B). These results suggest a difference in the capacity of acquiring or processing particulate antigens for HLA class II presentation between the 2 DC subsets, as suggested previously.15
Activation of anti–influenza virus CD8+ CTL memory responses by pDCs and CD11c+ DCs
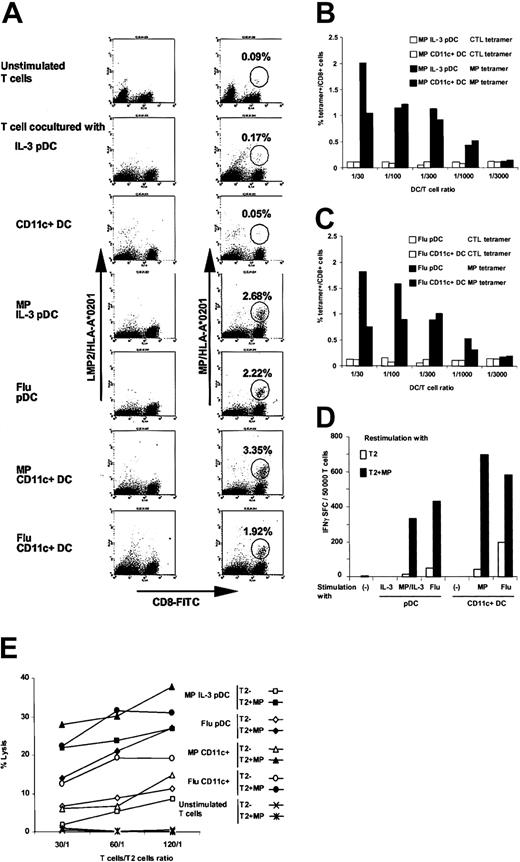
The majority of HLA-A*0201+ individuals have a strong memory CTL response against influenza MP(58-66). Upon re-exposure to influenza virus, this memory CTL response is rapidly activated. Mature CD11c+ DCs are one of the most efficient APCs to activate this response, whereas monocytes are quite inefficient.13 17 To test whether pDCs have the capacity to activate memory cells, T cells from HLA-A*0201+ donors were cultured in vitro with autologous pDCs or CD11c+ DCs previously pulsed with influenza MP(58-66) peptide or influenza virus. After a week, expansion of HLA-A*0201–restricted influenza MP(58-66)–specific CTLs was assessed by PE-conjugated HLA-A*0201/peptide tetramer staining (Figure5A). A very low fraction of memory influenza MP(58-66)–specific CTLs was detected in T-cell populations cultured alone or with DCs not exposed to influenza antigens. In T-cell populations cocultured with pDCs or CD11c+ DCs previously pulsed with influenza MP(58-66), or infected with influenza virus, memory influenza MP(58-66)–specific CTLs were expanded at least 20-fold. This expansion was influenza antigen–specific since no staining was observed with a PE-conjugated HLA-A*0201/EBV LMP2 peptide tetramer used as a control. Although results varied from one experiment to another, pDCs cultured either with IL-3 and pulsed with peptide or exposed to influenza virus appeared to have a comparable ability to reactivate anti-influenza CTL memory responses with CD11c+DCs (Table 1).
Equivalent efficiency of pDCs and CD11c+ DCs to restimulate the HLA-A*0201–restricted influenza MP–specific CTL memory response.
T cells, pDCs, and CD11c+ DCs were purified from HLA-A*0201+ PBMCs. T cells were cocultured with pDCs or CD11c+ DCs infected by influenza virus or pulsed with influenza MP(58-66) peptide. (A) Then, 7 days later, the presence of HLA-A*0201–restricted MP-specific CD8+ T cells in the cocultures and in a frozen sample of unstimulated T cells was measured by staining with PE-conjugated tetrameric complexes of MP(58-66)/HLA-A*0201. A PE-conjugated tetrameric complex of LMP2/HLA-A*0201 was used as a control. (B) IL-3 pDCs or CD11c+ DCs pulsed with influenza MP(58-66)peptide were cocultured at 5 different DC/T-cell ratios. Then, 7 days later, the presence of HLA-A*0201–restricted MP-specific CTLs in the cultures was measured by tetramer staining. (C) pDCs or CD11c+ DCs infected by influenza were cocultured at 5 different DC/T-cell ratios. Then, 7 days later, the presence of HLA-A*0201–restricted MP-specific CTLs in the cultures was measured by tetramer staining. (D) Then, 7 days later, IFN-γ production by HLA-A*0201–restricted MP-specific CD8+ T cells in the cocultures and in a frozen sample of unstimulated T cells was assessed by IFN-γ ELISPOT using unpulsed or MP peptide–pulsed T2 as presenting cells. (E) Cytolytic activity of HLA-A*0201–restricted MP-specific CTLs in the cocultures and in a frozen sample of unstimulated T cells was assessed by 51Cr release assay using unpulsed or MP peptide–pulsed T2 cells as target cells.
Equivalent efficiency of pDCs and CD11c+ DCs to restimulate the HLA-A*0201–restricted influenza MP–specific CTL memory response.
T cells, pDCs, and CD11c+ DCs were purified from HLA-A*0201+ PBMCs. T cells were cocultured with pDCs or CD11c+ DCs infected by influenza virus or pulsed with influenza MP(58-66) peptide. (A) Then, 7 days later, the presence of HLA-A*0201–restricted MP-specific CD8+ T cells in the cocultures and in a frozen sample of unstimulated T cells was measured by staining with PE-conjugated tetrameric complexes of MP(58-66)/HLA-A*0201. A PE-conjugated tetrameric complex of LMP2/HLA-A*0201 was used as a control. (B) IL-3 pDCs or CD11c+ DCs pulsed with influenza MP(58-66)peptide were cocultured at 5 different DC/T-cell ratios. Then, 7 days later, the presence of HLA-A*0201–restricted MP-specific CTLs in the cultures was measured by tetramer staining. (C) pDCs or CD11c+ DCs infected by influenza were cocultured at 5 different DC/T-cell ratios. Then, 7 days later, the presence of HLA-A*0201–restricted MP-specific CTLs in the cultures was measured by tetramer staining. (D) Then, 7 days later, IFN-γ production by HLA-A*0201–restricted MP-specific CD8+ T cells in the cocultures and in a frozen sample of unstimulated T cells was assessed by IFN-γ ELISPOT using unpulsed or MP peptide–pulsed T2 as presenting cells. (E) Cytolytic activity of HLA-A*0201–restricted MP-specific CTLs in the cocultures and in a frozen sample of unstimulated T cells was assessed by 51Cr release assay using unpulsed or MP peptide–pulsed T2 cells as target cells.
Comparable expansion of HLA-A*0201-restricted influenza MP-specific CD8+ T by pDCs and CD11c+ DCs
| Experiment no. . | Unstimulated T cells . | Stimulated T cells . | |||
|---|---|---|---|---|---|
| MP IL-3 pDCs . | Flu pDCs . | MP CD11c+ DCs . | Flu CD11c+ DCs . | ||
| 1 | 0.09 | 2.68 | 2.22 | 3.35 | 1.92 |
| 2 | 0.07 | 0.82 | 0.63 | 1.17 | 0.69 |
| 3 | 0.05 | 1.19 | 3.87 | 4.64 | 3.62 |
| 4 | 0.07 | 0.49 | 0.78 | 1.15 | 0.88 |
| 5 | 0.03 | 0.08 | 0.36 | 0.08 | 0.18 |
| Experiment no. . | Unstimulated T cells . | Stimulated T cells . | |||
|---|---|---|---|---|---|
| MP IL-3 pDCs . | Flu pDCs . | MP CD11c+ DCs . | Flu CD11c+ DCs . | ||
| 1 | 0.09 | 2.68 | 2.22 | 3.35 | 1.92 |
| 2 | 0.07 | 0.82 | 0.63 | 1.17 | 0.69 |
| 3 | 0.05 | 1.19 | 3.87 | 4.64 | 3.62 |
| 4 | 0.07 | 0.49 | 0.78 | 1.15 | 0.88 |
| 5 | 0.03 | 0.08 | 0.36 | 0.08 | 0.18 |
T cells, pDCs, and CD11c+ DCs were purified from HLA-A*0201+ PBMCs. T cells were cocultured with pDCs or CD11c+ DCs infected with influenza virus or pulsed with influenza MP(58-66) peptide. Then, 7 days later, the presence of HLA-A*0201-restricted MP-specific CD8+ T cells in the cultures and in a frozen sample of unstimulated T cells was measured by flow cytometry using FITC-conjugated CD8 antibody and PE-conjugated MP(58-66)/HLA-A*0201 tetrameric complexes. Results were obtained with 5 different donors and are expressed as percent of MP tetramer+/CD8+ cells.
Since relatively low numbers of antigen-presenting CD11c+DCs are able to efficiently activate T cells,16,17 we wanted to determine if it was a property shared by pDCs. T cells were cocultured with different quantities of pDCs or CD11c+ DCs that had been pulsed with influenza MP(58-66) peptide or influenza virus. After a week, expansion of HLA-A*0201–restricted MP-specific T cells was measured by tetramer staining. Low numbers of pDCs (1 pDC for 1000 T cells) were as potent as the CD11c+DCs to reactivate the influenza-specific CTL memory response (Figure 5B-C). This result suggests that a few influenza virus–infected pDCs may be sufficient to expand these antiviral CTLs in vivo.
To assess cytokine production, the HLA-A*0201–restricted influenza MP(58-66)–specific CTLs expanded either by pDCs or CD11c+ DCs for one week were restimulated with T2 cells pulsed with influenza MP(58-66) peptide as antigen-presenting cells in an IFN-γ ELISPOT assay (Figure 5D). Influenza MP(58-66)–specific CTLs produced IFN-γ regardless of the source of antigen used to expand them (ie, peptide or influenza virus). In all experiments, the frequency of IFN-γ–producing CD8+ T cells correlated to the amount of cells detected by tetramer staining. Cytokine production by expanded CTLs was also analyzed by IL-4 and IL-10 ELISPOT assay. A few background spots were observed in response to unpulsed T2 cells, and no increase of this low number of spots was detected in response to influenza MP(58-66) peptide-pulsed T2 cells (data not shown).
A week after stimulation by pDCs and CD11c+ DCs, the cytolytic activity of the expanded influenza MP(58-66)–specific CTLs was analyzed using51Cr-labeled T2 cells as target cells. pDC- and CD11c+ DC–expanded CTLs showed a comparable antigen-specific cytolytic activity (Figure 5E). A higher nonspecific response to unpulsed T2 cells was observed for the CTL population expanded by influenza virus–infected CD11c+ DCs. This nonspecific response was also observed in the IFN-γ ELISPOT assays (Figure 5D).
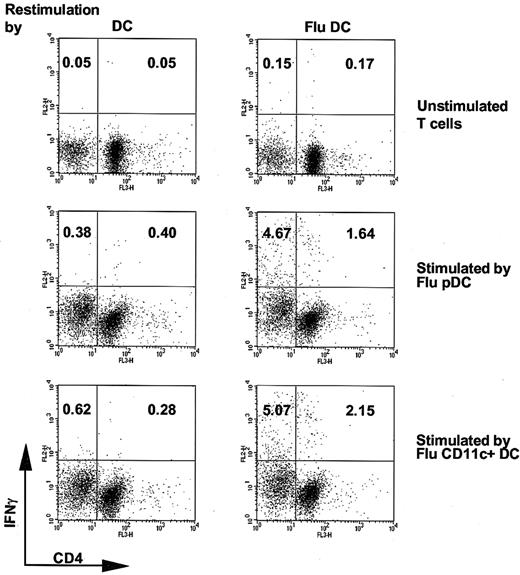
Activation of anti–influenza virus CD4+ T-cell memory responses by pDCs and CD11c+ DCs
We next determined if pDCs could also activate the anti-influenza CD4+ T-cell memory response. T cells were cultured with autologous pDCs or CD11c+ DCs previously cultured with influenza virus. After a week, expansion of influenza virus–specific CD4+ T cells was assessed by IFN-γ, IL-4, and IL-10 intracytoplasmic staining using mature monocyte-derived DCs infected by influenza virus as APCs (Figure 6). IFN-γ–producing CD4+ T cells were observed in populations stimulated either by influenza virus–infected pDCs or CD11c+ DCs. No influenza virus–specific CD4+ T cells were detected in the unstimulated T-cell population. Furthermore, expansion of influenza virus–specific CD4− T cells was also observed (likely to be CD8+ T cells), and this population was consistently larger than the influenza virus–specific CD4+ T cells in all experiments. No antigen-specific production of IL-4 and IL-10 was observed. Collectively, these results show that after exposure to influenza virus, pDCs efficiently activate TH1 CD4+ and CD8+ CTL anti-influenza memory responses.
Equivalent efficiency of influenza virus–infected pDCs and CD11c+ DCs to activate influenza A virus Aichi/68 memory CD4+ T-cell response.
T cells were cocultured with pDCs or CD11c+ DCs infected by influenza virus. After 7 days, T cells were restimulated by autologous monocyte-derived mature DCs infected or not with influenza virus in the presence of brefeldin-A. Production of IFN-γ by CD4+ T cells was assessed by intracytoplasmic staining and flow cytometry.
Equivalent efficiency of influenza virus–infected pDCs and CD11c+ DCs to activate influenza A virus Aichi/68 memory CD4+ T-cell response.
T cells were cocultured with pDCs or CD11c+ DCs infected by influenza virus. After 7 days, T cells were restimulated by autologous monocyte-derived mature DCs infected or not with influenza virus in the presence of brefeldin-A. Production of IFN-γ by CD4+ T cells was assessed by intracytoplasmic staining and flow cytometry.
Discussion
Until now, evidence that pDCs contribute to the induction of adaptive antiviral immune responses has been only indirect. To the best of our knowledge, our studies provide the first demonstration of the capacity of pDCs to process and present influenza antigens, leading to the activation of virus-specific CTLs and TH1 CD4+ T cells. Furthermore, our studies confirm previous findings that pDCs exposed to influenza virus produce IFN-α; mature (as manifested by the up-regulation of CCR7; the expression of the maturation-associated marker CD83; and the heightened expression of costimulatory and HLA molecules and their capacity to migrate toward CCL19); and are resistant to virus-induced apoptosis.7 8
Strikingly, pDCs are comparable to CD11c+ DCs in their capacity to activate T-cell responses. This was apparent at several levels. Both DC subsets activated Th1 CD4+ T cells and IFN γ–producing cytolytic CD8+ T cells. The responses were quantitatively similar as determined by intracellular cytokine staining, IFN-γ ELISPOT, and the frequency of tetramer-binding MP reactive cells. Furthermore, the reactivation of influenza-specific memory responses did not require the addition of exogenous cytokines and required relatively few DCs. The only noted difference with respect to viral antigen presentation was the inability of pDCs to present boiled influenza virus to CD4+ T cells. Boiled virus lacks intact envelope, suggesting that envelope-membrane interactions may be essential for viruses to be internalized by pDCs.
Given their advantage over myeloid DCs to produce type I interferons and maintain survival through constitutive expression of MxA, we speculate that pDCs play a primary role in the innate and adaptive response to influenza virus, indeed, probably many enveloped viruses. For instance, herpes, Sendai, and HIV-1 viruses all induce the production of type I interferons from pDCs.4-7 The critical role of pDCs in the initiation of innate immunity and antiviral T-cell responses may explain why the reconstitution of the pDC subset in HIV+ patients during antiretroviral therapy correlates with resistance to opportunistic infections.18Animal models have also demonstrated that intact pDC function is essential for resistance to murine cytomegalovirus.19
The chemokine receptor expression by pDCs as well as their localization in vivo are in accordance with the concept that pDCs participate in the cellular immune responses to viruses. Immature pDCs, like immature CD11c+ DCs, express chemokine receptors (eg, CCR5, CXCR3) corresponding to inflammatory cytokines (eg, CCL5, CXCL10). They may be attracted to inflammatory sites in vivo, even if in vitro they do not migrate in response to these inflammatory chemokines.10For instance, accumulation of pDCs has been observed in pathologic tissues from subjects with granulomatous lymphadenitis,20Kukichi lymphadenitis,21 epithelioid cell granulomas,22 cutaneous manifestations of systemic lupus erythematosus,23 and in nasal mucosa during allergic reactions.24 At the site of inflammation, pDCs along with their myeloid DC counterparts may conceivably capture antigens through direct infection or cross presentation, while receiving additional stimuli that promote maturation (eg, TNF-α, IL-1, and IL-6 produced by virus-infected monocytes; CD40-L expressed by activated platelets and mastocytes; and influenza virus). Once mature, both pDCs and myeloid DCs up-regulate CCR7 expression allowing them to migrate to lymph nodes, where they can participate in the initiation of antigen-specific T-cell responses.10,11 pDCs clearly have the capacity to stimulate resting memory cells, as demonstrated here. Because pDCs accumulate in inflammatory sites, they may have the capacity to stimulate memory T cells directly in tissues (ie, “effector memory T cells”) and, after CCL19-driven migration to the lymph node, stimulate central memory T cells and naive T cells.25 Further studies are under way to ascertain the role pDCs play in stimulating these T-cell subsets.
pDCs, like myeloid DCs, demonstrate a plasticity that is regulated by their microenvironment. Depending on the circumstances, they can induce CD4+ helper T-cell responses, cytolytic CD8+effectors, NK T cells, and even anergic, immunosuppressive T-cell populations.7,8,26,27 pDCs exposed to virus (HSV, influenza virus) induce TH1 T-cell responses, characterized by IFN-γ production, whereas pDCs exposed to IL-3 induce TH2 responses.7,26 Furthermore, freshly isolated pDCs or pDCs cultured with either IL-3 or influenza virus can induce subsets of T cells to produce IL-10, a cytokine with immunosuppressive effects on T-cell responses.7,8 27 In our study, we detected only TH1 responses among the influenza virus antigen–specific T cells stimulated either by pDCs exposed to IL-3 or influenza virus. IL-10 was not detected in responding T cells, probably because we studied a memory response.
Besides their role as APCs, the cytokines and chemokines produced by pDCs exposed to viruses would exert significant autocrine and paracrine effects in their microenvironments. Influenza virus induces the production of CXCL8, CXCL10, CCL3, and CCL5 by pDCs, a panel of chemokines also produced by CD11c+ DCs. This virus-specific induction of chemokines may recruit additional pDCs, CD11c+DCs, and monocytes, as well as other cells, into inflammatory lesions. Type I IFNs released by pDCs would inhibit viral infection of neighboring cells; promote the induction of activated CD8+and CD4+ T cells into CTLs and TH1 helper CD4+T cells, respectively; and may even induce the differentiation of DCs from monocytes.28-30
The central issue raised by our studies is whether pDCs can provide a protective function at the level of T cells in chronic viral infection. Given that pDCs are depleted in HIV-1 infection when viral loads are high and CD4 counts are low, it may be useful to consider their mobilization in vivo via factors such as flt-3 ligand or intervention with antigen-pulsed combinations of pDCs and CD11c+ DCs. Indeed it is now feasible to separate these subsets for clinical use, so direct comparisons of the 2 populations will be feasible in the future. Along these lines, the identification of the murine counterpart of pDCs31-33 will elucidate the relationships and function of these cells.
The authors thank Klara Velinzon and Svetlana Mazel for technical expertise.
Prepublished online as Blood First Edition Paper, January 2, 2003; DOI 10.1182/blood-2002-10-3063.
Supported by the National Institutes of Health (NIH) grants AI 44628 and AI 39516 to N.B. and MOI-RR00102 to the Rockefeller University Clinical Research Center; a Burroughs Wellcome Clinical Investigator grant; and Elizabeth Glaser and Doris Duke Foundation Awards to N.B. Funding was also provided by the Academic Medicine Development Company (AMDeC) Foundation of New York City through its “Tartikoff/Perelman/EIF Fund for Young Investigators in Women's Cancers” to M.L. and the ARC (Association Pour la Recherche sur le Cancer) to J.F.F. C.M. is recipient of a Special Fellowship from the Leukemia & Lymphoma Society and of a grant from the Speaker's Fund for Public Health Research awarded by the city of New York.
J.-F.F. and M.G. contributed equally to this work.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Nina Bhardwaj, Laboratory of Molecular Neuro-Oncology, Rockefeller University, 1230 York Ave, New York, NY; e-mail: bhardwn@mail.rockefeller.edu.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal