The control of neutrophil turnover in the circulation is a key event in homeostasis and inflammation. Using CD18- deficient (CD18−/−) mice that show a 19-fold increase of blood neutrophil counts when compared with wild-type animals (CD18+/+), we found that apoptosis of peripheral neutrophils was significantly reduced from 27.4% in the wild-type to 4.8% inCD18−/− mice within 4 hours after isolation as measured by analysis of DNA content. This was confirmed by detecting CD16 expression, nuclear morphology, and internucleosomal DNA degradation. In contrast, no difference in apoptosis was observed in neutrophils derived from the bone marrow. Neutrophilia and delayed neutrophil apoptosis were also present inCD18−/−/interleukin 6 (IL-6−/−) double knockout mice. Moreover, plasma ofCD18−/− mice was not able to delay apoptosis of CD18+/+neutrophils and plasma ofCD18+/+ mice did not augment apoptosis of CD18−/−neutrophils. However,CD18−/− neutrophils revealed an up-regulation of the antiapoptotic gene bcl-Xl and a down-regulation of the proapoptotic gene bax-α compared withCD18+/+ neutrophils suggesting that this delayed apoptosis. Accordingly, down-regulation of Bax-α using antisense technique delayed apoptosis and prolonged neutrophil survival. The replacement of the hematopoietic system of CD18+/+ mice by a 1:1 mixture of CD18+/+ andCD18−/− hematopoietic cells abolished the delay of apoptosis in peripheralCD18−/− neutrophils and prevented neutrophilia. Altogether, this suggests that a delay of neutrophil apoptosis inCD18−/− mice causes an alteration of neutrophil homeostasis, which may induce the massive increase of peripheral neutrophil counts. Thus, apoptosis seems to be critically involved in the control of neutrophil turnover in the circulation.
Introduction
Apoptosis (programmed cell death) represents the key mechanism for the controlled elimination of cells within the body and thus contributes to the maintenance of tissue homeostasis by helping to keep the balance between cell proliferation and cell death. Apoptosis is an active and well-regulated process that is characterized by specific phenomena such as cell shrinkage, chromatin condensation, internucleosomal DNA fragmentation, membrane blebbing, and finally the decay into apoptotic bodies.1,2 Human polymorphonuclear neutrophils (PMNs) die spontaneously by apoptosis within hours to days but their lifetime can be shortened or extended by modulating apoptosis.3 Several inflammatory cytokines are known to affect PMN apoptosis in vitro. The proinflammatory mediator tumor necrosis factor α (TNF-α), for example, is known to reduce the life span of human PMNs by accelerating apoptosis.4 Other cytokines such as granulocyte-macrophage colony-stimulating factor (GM-CSF) and granulocyte colony-stimulating factor (G-CSF) promote PMN survival by inhibiting apoptosis.5 The intracellular mechanism that controls the apoptotic machinery in PMNs subsequent to cytokine stimulation involves the Bcl-2 family of apoptosis-associated genes, which consists of antiapoptotic (Bcl-2, Bcl-Xl, Mcl-1, A1, etc) and proapoptotic members (Bax-α, Bak, Bad, Bcl-Xs, Bik, etc).6 The shift of the balance between the proapoptotic factor Bax-α and the antiapoptotic factor Bcl-Xl toward the proapoptotic gene product is known to promote apoptosis of human PMNs.4 7
In the situation in vivo, apoptosis of PMNs in the tissue is thought to be critical for the final resolution of acute inflammation because it prevents the uncontrolled release of their proinflammatory contents and allows the nonphlogistic elimination of PMNs by macrophages and other tissue cells.8-10 However, in addition to PMN infiltration of the tissue, the acute inflammatory response is accompanied by an expansion of the peripheral PMN pool that is generally believed to be due to an enhanced PMN production and maturation in the bone marrow—an effect that is mediated by cytokines such as G-CSF and GM-CSF.11 However, several reports suggest that inflammation-mediated neutrophilia is not simply due to enhanced hematopoiesis. In patients with severe burns, circulating PMNs showed impaired apoptosis that was induced by plasma factors up-regulating GM-CSF levels.12 Cytokine-mediated delay of apoptosis in peripheral PMNs was also observed in other inflammatory diseases associated with neutrophilia such as cystic fibrosis and pneumonia.7 Moreover, neutropenia in myelokathexis, a congenital disorder, has been reported to involve a modulation, that is, an enhancement of PMN apoptosis, which was associated with a down-regulation of the antiapoptotic gene product Bcl-Xl.13 Thus, a body of evidence indicates that the dysregulation of PMN apoptosis may contribute to the expansion or the reduction of the peripheral PMN pool under pathologic conditions. Together, this supports the concept that the control of PMN apoptosis is not only involved in the final resolution of inflammation by terminating the lifetime of the emigrated PMNs in the tissue and allowing their final elimination, but also seems to be critical for the modulation of the peripheral PMN count—at least under pathophysiologic conditions. At least under pathophysiologic conditions, apoptosis seems to be critical for the modulation of the peripheral PMN count. However, little is known about the mechanisms that contribute to the maintenance of PMN homeostasis under normal, noninflammatory conditions.
To address the question whether apoptosis may contribute to the homeostasis of the functional PMN pool in the circulation under noninflammatory conditions, we analyzed apoptosis of PMNs in an animal model using CD18-deficient (CD18−/−) mice and wild-type (CD18+/+) mice with the same genetic background as well as CD18/interleukin 6 double knockout (CD18−/−/IL-6−/−) mice. In addition, PMN apoptosis was studied inCD18+/+/CD18−/−chimeric mice in which the hematopoietic system was replaced by a 1:1 mixture of CD18+/+ andCD18−/− hematopoietic cells. Apoptosis was detected by measurement of CD16 expression on the cell surface by analysis of DNA content and nuclear morphology as well as by detection of DNA degradation (DNA-ladder). The role of the bcl-2 family of apoptosis-associated genes was investigated by semiquantitative reverse transcription–polymerase chain reaction (RT-PCR) and by studying PMN apoptosis in the presence of antisense oligonucleotides.
Materials and methods
Isolation of murine PMNs
Murine PMNs were isolated from mutant mice deficient in CD18 or wild-type control animals of the same genetic background (mixed 129/Sv and C57BL/6J). In addition, CD18/IL-6 double-knockout mice and wild-type animals with the same genetic background were used (mixed 129/Sv and C57BL/6J). All mice have been genotyped by Southern blot analysis as described previously14 and were maintained under specific pathogen-free conditions in a barrier facility. Mice were used at the age of 14 to 20 weeks. At this time point, the animals were free of skin ulcerations and infections as measured by extended microbiologic screening. Animal experiments were institutionally approved. Peripheral blood was collected by resection of the tip of the tail, and aliquots of heparinized whole blood samples (200-700 μL) were incubated with the fluorescein isothiocyanate (FITC)–conjugated anti–Gr-1 monoclonal antibody (mAb; final concentration 10 μg/mL) for 30 minutes at 4°C. Blood was incubated for 1 minute with 2 mL lysis buffer (0.15 M NH4Cl, 1 mM KHCO3, and 0.1 mM EDTA [ethylenediaminetetraacetic acid) at room temperature and washed twice with 10 mL phosphate-buffered saline (PBS)–buffer (PBS supplemented with 2 mM EDTA and 0.5% bovine serum albumin [BSA]). Subsequently, samples (107 leukocytes) were incubated for 20 minutes at 10°C with 10 μL magnetic beads coupled to a monoclonal mouse anti-FITC antibody (anti-FITC microbeads, Miltenyi Biotec, Bergisch Gladbach, Germany) and 90 μL PBS-buffer. Cell separation was performed according to the supplier's protocol. Briefly, after washing with PBS-buffer, cells were suspended in 500 μL PBS-buffer and loaded onto MACS MS separation columns (Miltenyi Biotec) for magnetic separation. The column was washed 3 times with 1 mL PBS-buffer and was removed from the separator. Samples were eluted twice by addition of 5 mL PBS-buffer. For isolation of PMNs from the bone marrow, animals were killed by CO2 inhalation and the bone marrow was harvested from tibias and femurs. Isolation of PMNs from the bone marrow was performed as described for PMN isolation from peripheral blood. Purity was more than 95% as measured by analysis of Gr-1+ cells using flow cytometry. Isolated PMNs were also analyzed for expression of CD18 to confirm the genotype (data not shown). After the isolation procedure, PMNs (5 × 106/mL) were cultured at 37°C in RPMI medium with HEPES (N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid) buffer supplemented with 10% fetal calf serum (FCS) unless indicated otherwise.
Separation of CD18+/+ andCD18−/− PMNs fromCD18+/+/CD18−/−chimeric mice
For separation of CD18+ andCD18− PMNs from the peripheral blood ofCD18+/+/CD18−/−chimeric mice, cells were treated with the FITC-conjugated anti–Gr-1 mAb as described (see “Isolation of murine PMNs”) and PMNs were isolated using the anti-FITC Multisort kit (Miltenyi Biotec). After isolation of PMNs, beads were released from the PMNs according to the supplier's instructions and PMNs were incubated for 15 minutes at 10°C with the phycoerythrin (PE)–labeled rat antimouse CD18 antibody C71/16 and CD18+/+, andCD18−/− PMNs were separated using magnetic beads coupled to a monoclonal mouse anti-PE antibody (anti-PE microbeads, Miltenyi Biotec) as described.
Generation ofCD18+/+/CD18−/−chimeric mice
Bone marrow cells were harvested fromCD18−/− and wild-type mice and transplanted into lethally irradiated wild-type mice as described previously.15 Recipient mice (8 weeks old) were lethally irradiated in 2 doses of 600 rads each approximately 4 hours apart. Bone marrow cells from donor mice were harvested by flushing both femurs and tibias with RPMI without phenol red (Gibco, Grand Island, NY) containing 10% FCS (Atlanta Biologicals, Norcross, GA) under sterile conditions. Suspended bone marrow cells were washed and erythrocytes were lysed in 0.15 M NH4Cl lysing solution. Approximately 4 million unfractionated bone marrow cells in 200 μL media were delivered intravenously through the tail vein of each recipient mouse. Recipient mice received transplants with a 1:1 mixture of CD18−/− and wild-type unfractionated bone marrow cells. Recipient mice were housed in a barrier facility (individually ventilated cages, high-efficiency particulate air [HEPA]) under pathogen-free conditions before and after bone marrow transplantation. After bone marrow transplantation, mice were maintained on autoclaved water with antibiotics (5 mM sulfamethoxazole, 0.86 mM trimethoprim; Sigma Chemical, St Louis, MO) and fed autoclaved food.
Analysis of DNA content
DNA content was analyzed by flow cytometry (FACScan, Becton Dickinson, Heidelberg, Germany) using propidium iodide (PI). Briefly, isolated PMNs (5 × 105/100 μL) were washed with PBS supplemented with 1 mM EDTA and resuspended in 70% ethanol. PMNs were permeabilized overnight at −20°C, washed with PBS supplemented with 1 mM EDTA, and suspended in 250 μL of the same buffer. After addition of 20 μg/mL RNAase and 50 μg/mL PI (final concentrations), samples were incubated for 15 minutes at room temperature and kept at 4°C until flow cytometric analysis. In each sample, 104 cells were counted and analyzed using Cell Quest software (Becton Dickinson).
Cell surface expression of CD16
For analysis of CD16 expression of PMNs derived fromCD18+/+ orCD18−/− mice, aliquots of whole blood (10-40 μL) were incubated for 1 hour at 4°C in the dark with the PE-conjugated anti-CD16 mAb (final concentration of 10 μg/mL). Subsequently, samples were treated for 10 minutes in the dark with 500 μL fluorescence-activated cell sorting (FACS) lysing solution (Becton Dickinson), washed twice with PBS supplemented with 1 mM EDTA, and subjected to flow cytometry. In each sample, 104 cells were counted, gated off-line for granulocytes, and analyzed using Cell Quest software. For analysis of CD16 expression of PMNs derived fromCD18+/+/CD18−/−chimeric mice, aliquots of whole blood (80-100 μL) were stained with the PE-conjugated anti-CD18 mAb (final concentration of 10 μg/mL) and the FITC-labeled anti-CD16 mAb (final concentration of 10 μg/mL) and treated as described.
Analysis of nuclear morphology
Isolated PMNs were treated with acridine orange in a final concentration of 5 μg/mL for 5 minutes at room temperature and investigated on a Nikon fluorescence microscope using an epifluorescence adapter (Nikon DM510, B-2A; Duesseldorf, Germany) and an 40/0.6 objective.
Internucleosomal DNA fragmentation assay
Isolated PMNs (107) from several mice (3-7) were pooled after culture and lysed for 10 minutes on ice in 600 μL hypotonic lysis buffer (10 mM EDTA, 0.2% Triton X-100, 10 mM Tris [tris(hydroxymethyl)aminomethane], pH 7.5). After centrifugation for 10 minutes at 4°C at 13 000g, DNA was isolated by phenol/chloroform extraction and subsequent precipitation with 2.5 volumes ethanol containing 0.1 M NaCl overnight at −20°C. After centrifugation at 13 000g, the pellets were washed in 1 mL 70% ethanol, dried, and suspended in 20 μL H20. After treatment with DNase-free RNase in a final concentration of 0.8 mg/mL for 30 minutes at 37°C, samples were analyzed by gel electrophoresis in 1.8% agarose and visualized by ethidium bromide staining under UV light.
RT-PCR
For isolation of RNA, about 600 μL blood was collected fromCD18+/+ mice that yielded about 1 million PMNs after isolation using the magnetic bead separation technique. About 20 million PMNs were obtained from an equal volume of blood from CD18−/− mice. Total RNA was isolated by the guanidine isothiocyanate method16 using Trizol (Life Technologies, Eggenstein, Germany), which yielded about 250 ng total RNA per 1 million PMNs. An aliquot of 50 ng RNA was transcribed into cDNA using oligo(dT) primers (Amersham Pharmacia Biotech, Freiburg, Germany) and 50 U reverse transcriptase Moloney murine leukemia virus (MMLV; Promega, Madison, WI). PCR amplification was carried out using specific primer sets (TIB MOLBIOL, Berlin, Germany) for bcl-X (upstream primer: 5′-TTG-GAC-AAT-GGA-CTG-GTT-G; downstream primer: 5′-GTC-TGG-TCA-CTT-CCG-ACT-GA, 746-bp product); bax-α (upstream primer: 5′-CTG-AGC-AGA-TCA-TGA-AGA-CAG-G; downstream primer: 5′-CAG-TTG-AAG-TTG-CCG-TCA-G, 274-bp product), A1 (upstream primer: 5′-GAT-GGC-TGA-GTC-TGA-GCT-CA; downstream primer: 5′-GGC-AAT-CTG-CTC-TTG-TGG-AA, 330-bp product), bad (upstream primer: 5′-ATG-TTC-CAG-ATC-CCA-GAG-TT; downstream primer: 5′-TCA-CTG-GGA-GGG-GGC-GGA-GC, 490-bp product), and bak (upstream primer: 5′-TGA-AAA-ATG-GCT-TCG-GGG-CAA-GGC; downstream primer: 5′-GTG-AAG-AGT-TCG-TAG-GCA-TT, 332-bp product). For control, a specific primer set for β-actin (upstream primer: 5′-ATG-GCC-ACT-GCC-GCA-TCC-TC; downstream primer: 5′-CTA-GAA-GCA-CTT-GCG-GTG-CA, 430-bp product) was used. PCR (30 [β-actin] or 35 [others] cycles: 55 seconds 94°C, 55 seconds 60°C, 55 seconds 72°C) was performed using 1.25 U AmpliTaq DNA polymerase (Perkin Elmer, Weiterstadt, Germany). PCR products were analyzed by agarose gel electrophoresis and visualized with ethidium bromide under UV light.
Antisense experiments
Isolated PMNs (5 × 106/mL) were incubated with a mixture of 2 different bax antisense or scrambled oligonucleotides as described previously for down-regulation of human bax.7The sequence was adapted according to the murine gene sequence, and oligonucleotides with a phosphorothioate backbone were used. (antisense 1: 5′-TCG-ATC-CTG-GAT-GAA-ACC-CT; antisense 2: 5′-TCC-CCA-GCC-ATC-CTC-CCT-GC; scrambled 1: 5′-TCA-GTC-CTG-GTA-GAA-CAC-CT; scrambled 2: 5′-CTC-ACC-CCA-CTT-CGC-CTC-GC). PMNs were treated with the oligonucleotides in a final concentration of 20 μM each at 37°C in RPMI medium without addition of FCS for the first 60 minutes of culture to increase uptake of the oligonucleotides.
Detection of Bax-α expression
After treatment with antisense or scrambled oligonucleotides as described for antisense experiments, PMNs (5 × 105) were permeabilized overnight at −20°C in 70% ethanol. After washing with PBS supplemented with 1 mM EDTA, PMNs were suspended in 20 μL PBS supplemented with 1 mM EDTA and were incubated with the polyclonal anti-Bax antibody in a final concentration of 10 μg/mL for 20 minutes at 4°C. After washing twice, samples were incubated with a FITC-conjugated goat antirabbit IgG for 20 minutes at 4°C. After 2 washes, samples were subjected to flow cytometry (FACScan, Becton Dickinson) and 104 cells were counted and analyzed using Cell Quest software.
Antibodies
The PE-labeled rat antimouse CD18 antibody (clone C71/16), the FITC-labeled rat antimouse Gr-1 antibody (clone RB6-8C5), the PE- and the FITC-conjugated rat antimouse CD16 antibody (clone 2.4G2), and the PE-conjugated rat antimouse CD14 antibody (clone rmC5-3) were obtained from Pharmingen (San Diego, CA). The polyclonal anti-Bax antibody (N-20) was obtained from Santa Cruz Biotechnology (Santa Cruz, CA). The FITC-conjugated goat antirabbit IgG was purchased form Sigma (Deisenhofen, Germany). The polyclonal goat antimouse G-CSF antibody and the control goat IgG were obtained from R & D Systems (Wiesbaden-Nordenstadt, Germany).
Reagents
Acridine orange (3,6-Bis-(dimethyl-amino)-acridine), BSA, DNase-free RNase, ethidium bromide, penicillin, PI, RNase A, streptomycin, and Triton X-100 were obtained from Sigma (Deisenhofen, Germany). Buffers, cell culture media, and FCS were obtained from Biochrom (Berlin, Germany). The gyrase inhibitor Baytril containing 25 mg/mL enrofloxacin was obtained from Bayer (Leverkusen, Germany). The bax-α antisense and scrambled oligonucleotides were obtained from TIB MOLBIOL. The enzyme-linked immunosorbent assay (ELISA) kits (KMC2011 for mouse GM-CSF and KMC4021 for mouse interferon-γ [IFN-γ]) were purchased from Biosource (Ratingen, Germany).
Statistical analysis
Data shown represent mean ± SD where applicable. Statistical significance was determined using the Studentt test.
Results
Alteration of blood PMN homeostasis inCD18−/− mice
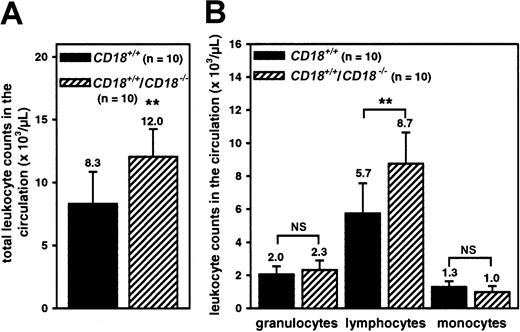
The analysis of leukocyte counts in the peripheral blood ofCD18−/− mice and wild-type control animals (Figure 1A) showed that total leukocyte counts were about 9-fold elevated in the deficient animals (84.2 × 103/μL) compared with wild-type controls (9.6 × 103/μL), a result that is in accordance with previous observations.14 17 This effect was largely due to neutrophilia with about a 19-fold increase of granulocytes from 3.1 × 103/μL in wild-type controls to 58.0 × 103/μL inCD18−/− mice (Figure 1B). However, lymphocyte counts (3.5-fold) as well as monocyte counts (11-fold) were elevated in the gene-deficient animals compared with controls. Although extended microbiologic screening had shown that the animals used had no infections (data not shown), we studied the effect of the antibiotic enrofloxacin on the leukocyte counts. A final concentration of 0.01% enrofloxacin in the drinking water over 13 days slightly diminished the PMN counts in the circulation of the mutant mice (n = 4) as measured at day 2, 5, 7, and 13 of enrofloxacin treatment (data not shown). However, the effect was not significant and PMN counts remained several-fold elevated when compared with enrofloxacin-treated control animals (n = 8). Moreover, PMN counts in the wild-type animals were slightly reduced in the presence of enrofloxacin. Together, this may further confirm that the increase of leukocyte counts in the absence of CD18 was not due to the activation of host defense mechanisms caused by bacterial infections.
Neutrophilia inCD18−/− mice.
Total (A) and differential leukocyte counts (B) in whole blood samples obtained from CD18+/+(n = 23) or CD18−/− mice (n = 21). Data represent means ± SDs; **P < .001.
Neutrophilia inCD18−/− mice.
Total (A) and differential leukocyte counts (B) in whole blood samples obtained from CD18+/+(n = 23) or CD18−/− mice (n = 21). Data represent means ± SDs; **P < .001.
Delayed apoptosis of blood PMNs inCD18−/− mice
To prove the hypothesis that a delay of apoptosis may contribute to the massive accumulation of neutrophils in the circulation, we measured the loss of DNA content, a well known marker of apoptosis,1 in PMNs that were isolated from the circulation of CD18−/− orCD18+/+ animals. Figure2A shows the data obtained in one representative experiment. Within 4 hours after the onset of culture, the original fluorescence histogram revealed a decrease of the gDNA content in 27.8% of PMNs derived from the circulation of wild-type mice, whereas only 3.4% of mutant PMNs showed a loss of DNA content within the same time period. Figure 2B shows the mean values of the observed effect in PMNs from 7CD18+/+ mice and 5CD18−/− mice. The quantitative analysis revealed that 0.8% of PMNs freshly isolated from the circulation of wild-type animals (0 hours) showed a loss of DNA content. In contrast, only 0.2% of the PMNs derived from the circulation of mutant mice were apoptotic. Within 4 hours after the onset of culture of the freshly isolated PMN, 27.4% of wild-type cells underwent apoptosis, whereas only 4.8% of the PMNs isolated from the circulation of CD18−/− mice showed a loss of DNA content. This corresponds to a reduction of apoptosis in absence of CD18 to 17.5% compared with wild-type controls (100%). To confirm this observation, we measured the down-regulation of CD16 (Fcγ receptor type III) expression on the cell surface as a marker for PMN apoptosis in whole blood samples.18 Figure3A shows one representative fluorescence histogram of the results obtained. When aged in culture for 8 hours, 30.1% of PMNs obtained from the circulation of wild-type animals showed a decrease of CD16 expression on the cell surface. In contrast, only 6.8% of PMNs from mutant mice had a substantially reduced CD16 expression. Figure 3B shows the mean values obtained from 13 wild-type animals and 11 CD18-deficient mice. The data revealed that 5.4% of PMNs freshly isolated from the circulation (0 hours) of wild-type animals showed low CD16 expression on the cell surface. In contrast, only 0.6% of PMNs from the mutant mice revealed diminished CD16 expression. Similar results were obtained at later time points (4, 8, and 22 hours after the onset of culture) with 13.1%, 32.3%, and 65.7% of PMNs with low CD16 expression in the wild-type and 1.4%, 8.7%, and 42.4% of PMNs showing reduced CD16 expression in the absence of CD18. Thus, the delay of neutrophil apoptosis was not only detectable in isolated PMNs but also in PMNs of whole blood samples, demonstrating that the observed effect was not due to the isolation procedure.
A delay of apoptosis in blood PMNs ofCD18−/− mice.
Flow cytometric analysis of DNA content measured in propidium iodide–stained PMNs isolated from the circulation ofCD18+/+ (n = 7) orCD18−/− mice (n = 5). (A) Representative recording of the fluorescence histograms obtained from isolated blood PMNs aged for 4 hours in culture without further stimulation. Numbers indicate apoptotic PMNs in percent of total cell number. (B) Mean values obtained after 0 hours and 4 hours of culture. Data represent means ± SDs; **P < .005.
A delay of apoptosis in blood PMNs ofCD18−/− mice.
Flow cytometric analysis of DNA content measured in propidium iodide–stained PMNs isolated from the circulation ofCD18+/+ (n = 7) orCD18−/− mice (n = 5). (A) Representative recording of the fluorescence histograms obtained from isolated blood PMNs aged for 4 hours in culture without further stimulation. Numbers indicate apoptotic PMNs in percent of total cell number. (B) Mean values obtained after 0 hours and 4 hours of culture. Data represent means ± SDs; **P < .005.
Delayed apoptosis of PMNs inCD18−/− mice is also apparent in whole blood samples.
Flow cytometric analysis of CD16 expression on the cell surface of PMNs using the PE-labeled anti-CD16 mAb measured in whole blood samples obtained from CD18+/+(n = 13) or CD18−/− mice (n = 11). (A) Representative recording of the fluorescence histograms obtained from PMNs aged for 8 hours in culture without further stimulation. Numbers indicate apoptotic PMNs with low CD16 expression in percent of total cell number. (B) Mean values obtained after 0, 4, 8, or 22 hours of culture. Data represent means ± SDs; **P < .005.
Delayed apoptosis of PMNs inCD18−/− mice is also apparent in whole blood samples.
Flow cytometric analysis of CD16 expression on the cell surface of PMNs using the PE-labeled anti-CD16 mAb measured in whole blood samples obtained from CD18+/+(n = 13) or CD18−/− mice (n = 11). (A) Representative recording of the fluorescence histograms obtained from PMNs aged for 8 hours in culture without further stimulation. Numbers indicate apoptotic PMNs with low CD16 expression in percent of total cell number. (B) Mean values obtained after 0, 4, 8, or 22 hours of culture. Data represent means ± SDs; **P < .005.
To confirm the delay of PMN apoptosis inCD18−/− mice, we studied the morphology of the nuclei by fluorescence microscopy after acridine orange staining (Figure 4A). Almost all PMNs isolated from the circulation of wild-type animals showed highly condensed nuclei (arrows) within 4 hours after the onset of culture, which is typical for apoptotic PMNs. In contrast, the majority of PMNs from CD18−/− mice showed segmented nuclei within this time period, which is typical for mature, nonapoptotic PMNs and only some PMNs showed condensation of the nuclei. Next, the degradation of gDNA was studied (Figure 4B). And again, only PMNs derived from wild-type animals showed strong DNA laddering within 4 hours after the onset of culture, whereas this effect was barely detectable in PMNs derived fromCD18−/− mice. Thus, we were able to demonstrate a substantial delay of PMN apoptosis in the peripheral blood of CD18−/−mice compared with PMNs from wild-type control animals by the use of 4 independent methods.
Analysis of nuclear morphology and DNA degradation.
(A) Epifluorescence photomicrographs of isolated blood PMNs fromCD18+/+ mice orCD18−/− mice stained with acridine orange 4 hours after the onset of culture. Results are representative of 3 independent experiments. (B) Agarose gel of low-molecular-weight DNA of isolated blood PMNs fromCD18+/+ orCD18−/− mice 4 hours after the onset of culture. Results are representative of 3 independent experiments.
Analysis of nuclear morphology and DNA degradation.
(A) Epifluorescence photomicrographs of isolated blood PMNs fromCD18+/+ mice orCD18−/− mice stained with acridine orange 4 hours after the onset of culture. Results are representative of 3 independent experiments. (B) Agarose gel of low-molecular-weight DNA of isolated blood PMNs fromCD18+/+ orCD18−/− mice 4 hours after the onset of culture. Results are representative of 3 independent experiments.
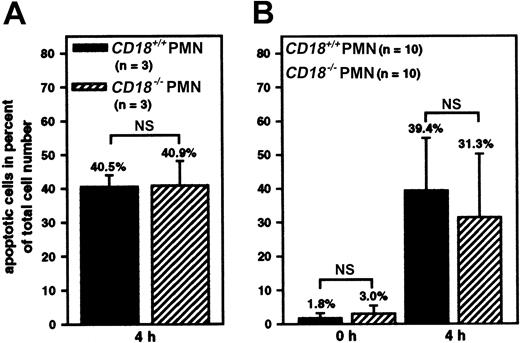
To find out whether the observed delay of apoptosis in the peripheral PMNs was due to an effect that was already induced in the bone marrow prior to the release of the PMNs into the circulation, apoptosis was studied in PMNs isolated from the bone marrow. Using PMNs derived from 6 CD18-deficient animals and 5 wild-type mice, no significant difference in apoptosis was detectable by measuring the DNA content of isolated PMNs using propidium iodide (Figure5). This was true for freshly isolated PMN (0 hours) as well as for PMNs that were cultured for 4, 8, and 22 hours, respectively. Thus, the delay of apoptosis in the blood PMNs of the mutant mice was not a consequence of an effect in the bone marrow, demonstrating that the absence of CD18 has an impact on apoptosis not before PMNs are released into the circulation.
No difference of apoptosis in PMNs derived from the bone marrow.
Apoptosis as measured by detecting the loss of DNA content by flow cytometry using PI-stained PMNs isolated from the bone marrow ofCD18+/+ (n = 5) orCD18−/− mice (n = 6) after 0, 4, 8, or 22 hours of culture. Data represent means ± SDs; NS indicates not significant.
No difference of apoptosis in PMNs derived from the bone marrow.
Apoptosis as measured by detecting the loss of DNA content by flow cytometry using PI-stained PMNs isolated from the bone marrow ofCD18+/+ (n = 5) orCD18−/− mice (n = 6) after 0, 4, 8, or 22 hours of culture. Data represent means ± SDs; NS indicates not significant.
Because GM-CSF is postulated to cause neutrophilia in man by inhibiting apoptosis of PMNs,7 we studied the concentration of GM-CSF in the plasma ofCD18+/+ andCD18−/− mice by means of the ELISA technique (Figure 6). The analysis of the GM-CSF concentration showed that there was no significant difference in the concentration of GM-CSF in the plasma of both animal groups. Thus, an increase of the plasma levels of GM-CSF seems not to be involved in the delay of PMN apoptosis in the mutant mice. We also measured the concentration of IFN-γ in the plasma ofCD18+/+ andCD18−/− mice using an ELISA technique and found that it was below the detection limit of 1 pg/mL in both groups, suggesting that an increased IFN-γ level is not involved in the observed delay of apoptosis (data not shown). However, IL-6 is thought to promote PMN survival by inhibiting apoptosis,19and the plasma concentration of IL-6 has been previously reported to be elevated in CD18−/− mice when compared with wild-type control animals.14 Therefore, we analyzed the leukocyte counts in the peripheral blood of double-knockout mice that were deficient in both CD18 and IL-6 (CD18−/−/IL-6−/−mice). Similar toCD18−/− mice, theCD18−/−/IL-6−/−mice showed leukocytosis (Table 1). In contrast to CD18−/− mice, which revealed a massive neutrophilia as well as increased monocyte and lymphocyte counts, theCD18−/−/IL-6−/−mice showed only a neutrophilia but no increase of monocyte or lymphocyte counts when compared with the wild-type control animals. However, because neutrophilia was also present inCD18−/−/IL-6−/−mice, it seems rather unlikely that IL-6 alone is responsible for the observed effect in CD18−/−mice. Moreover, PMNs obtained from the circulation ofCD18−/−/ IL-6−/−mice showed also a significant delay of apoptosis when compared with PMNs from wild-type animals as measured by detecting the loss of CD16 expression on the cell surface as well as the DNA content (Table 2). Together, this shows that IL-6 is at least not required to induce the neutrophilia or the delay of PMN apoptosis in the animal models used.
Plasma concentrations of GM-CSF.
Plasma concentration of GM-CSF as measured by ELISA technique inCD18+/+ (n = 20) orCD18−/− mice (n = 14). Data represent means ± SDs; NS indicates not significant.
Plasma concentrations of GM-CSF.
Plasma concentration of GM-CSF as measured by ELISA technique inCD18+/+ (n = 20) orCD18−/− mice (n = 14). Data represent means ± SDs; NS indicates not significant.
Neutrophilia inCD18−/−/IL-6−/−mice
| . | Leukocyte counts, × 103/μL . | |||
|---|---|---|---|---|
| Total leukocytes . | Neutrophils . | Monocytes . | Lymphocytes . | |
| CD18+/+/IL-6+/+ (n = 12) | 14.1 ± 3.2 | 4.3 ± 1.2 | 2.1 ± 0.7 | 7.6 ± 2.1 |
| CD18−/−/IL-6−/− (n = 10) | 38.9 ± 8.2* | 28.9 ± 5.7* | 2.5 ± 1.1 | 5.5 ± 1.7 |
| . | Leukocyte counts, × 103/μL . | |||
|---|---|---|---|---|
| Total leukocytes . | Neutrophils . | Monocytes . | Lymphocytes . | |
| CD18+/+/IL-6+/+ (n = 12) | 14.1 ± 3.2 | 4.3 ± 1.2 | 2.1 ± 0.7 | 7.6 ± 2.1 |
| CD18−/−/IL-6−/− (n = 10) | 38.9 ± 8.2* | 28.9 ± 5.7* | 2.5 ± 1.1 | 5.5 ± 1.7 |
Shown are total and differential leukocyte counts in whole blood samples obtained fromCD18+/+/IL-6+/+mice andCD18−/−/IL-6−/−mice.
P < .001.
Delayed PMN apoptosis inCD18−/−/IL6−/−mice
| . | Apoptotic cells in percent of total cell number . | |
|---|---|---|
| CD16 expression . | DNA content . | |
| CD18+/+/IL-6+/+, n = 6 | ||
| 0 h | 26.6 ± 11.6 | 3.1 ± 1.0 |
| 4 h | 68.7 ± 5.8 | 19.7 ± 5.1 |
| CD18−/−/IL-6−/−, n = 5 | ||
| 0 h | 6.6 ± 3.9* | 0.6 ± 0.3† |
| 4 h | 19.1 ± 5.4† | 9.9 ± 2.3† |
| . | Apoptotic cells in percent of total cell number . | |
|---|---|---|
| CD16 expression . | DNA content . | |
| CD18+/+/IL-6+/+, n = 6 | ||
| 0 h | 26.6 ± 11.6 | 3.1 ± 1.0 |
| 4 h | 68.7 ± 5.8 | 19.7 ± 5.1 |
| CD18−/−/IL-6−/−, n = 5 | ||
| 0 h | 6.6 ± 3.9* | 0.6 ± 0.3† |
| 4 h | 19.1 ± 5.4† | 9.9 ± 2.3† |
Flow cytometric analysis of CD16 expression on the cell surface of PMNs measured in whole blood samples using the PE-labeled anti-CD16 mAb and flow cytometric analysis of DNA content of isolated PI-stained PMNs at 0 and 4 hours after the onset of culture. Data represent mean ± SD.
P < .01.
P < .001.
However, other plasma factors besides GM-CSF, IFN-γ, and IL-6 are known to cause a delay of PMN apoptosis.7 19 Therefore, we studied whether the plasma at all may have an effect on PMN apoptosis. PMNs freshly isolated from the circulation ofCD18+/+ mice orCD18−/− mice were incubated in the presence of plasma derived fromCD18+/+ orCD18−/− mice, respectively (Figure 7). It turned out that treatment of blood PMNs with plasma from both groups had absolutely no effect. Neither plasma derived from mutant mice was able to reduce apoptosis of wild-type PMNs when compared with apoptosis of wild-type PMNs treated with wild-type plasma nor was plasma from wild-type mice able to enhance apoptosis of mutant PMNs when compared with the effect of plasma from mutant mice. This suggests that soluble factors in the plasma were not sufficient to impair apoptosis of PMNs in CD18-deficient animals. However, we performed additional experiments in which G-CSF in plasma ofCD18−/− mice was neutralized using a goat antimouse G-CSF antibody. When compared with plasma alone or plasma in the presence of a goat control IgG, neutralizing G-CSF in plasma of CD18−/− mice had no effect on apoptosis of PMNs isolated from the peripheral blood of wild-type mice (data not shown). However, to further exclude the possibility that mutant mice have a soluble factor in the plasma that triggers a delay of apoptosis in mutant PMNs in the bone marrow, which might not have a detectable effect until the PMNs reach the circulation, we analyzed the effect of plasma from mutant mice on PMNs from the bone marrow of wild-type mice. However, this had no detectable effect on PMN apoptosis. Because bone marrow PMNs from wild-type animals did not respond to plasma from mutant mice with respect to a delay of apoptosis, this further supports the view that soluble factors in the plasma are probably not sufficient to delay PMN apoptosis in the absence of CD18.
Soluble factors in the plasma had no effect on PMN apoptosis.
Flow cytometric analysis of DNA content measured in PI-stained PMNs isolated from the circulation ofCD18+/+ mice (left),CD18−/− mice (middle), or the bone marrow of CD18+/+mice (right) in the presence of RPMI medium (without FCS) supplemented with 50% plasma from CD18+/+mice or CD18−/−mice. Data represent apoptotic cells in percent of apoptosis in the presence of wild-type plasma (100%) 8 hours after the onset of culture. Data represent means ± SDs; NS indicates not significant.
Soluble factors in the plasma had no effect on PMN apoptosis.
Flow cytometric analysis of DNA content measured in PI-stained PMNs isolated from the circulation ofCD18+/+ mice (left),CD18−/− mice (middle), or the bone marrow of CD18+/+mice (right) in the presence of RPMI medium (without FCS) supplemented with 50% plasma from CD18+/+mice or CD18−/−mice. Data represent apoptotic cells in percent of apoptosis in the presence of wild-type plasma (100%) 8 hours after the onset of culture. Data represent means ± SDs; NS indicates not significant.
Control of apoptosis by the bcl-2 family of apoptosis-associated genes
Next, we investigated the molecular mechanism that underlies the delay of PMN apoptosis in the circulation of CD18-deficient animals. Because the bcl-2 family of apoptosis-associated genes is critically involved in the control of apoptosis of human PMNs,4 we studied whether a shift of balance between proapoptotic and antiapoptotic members of this gene family may be also responsible for the delay of PMN apoptosis in vivo. Using semiquantitative RT-PCR, we found an up-regulation of the antiapoptotic factor bcl-Xland a down-regulation of the proapoptotic gene product bax-α in peripheral PMNs of mutant mice when compared with PMNs obtained from wild-type animals (Figure 8A). In contrast, no striking difference in the expression of A1, bad, or bak was observed between neutrophils fromCD18−/− animals when compared with control cells (data not shown) suggesting that the differential expression of these factors is not critical for the observed delay of apoptosis. However, to further characterize the shift of balance between bcl-Xl and bax-α, the bcl-Xl/bax-α ratio was calculated using the optical density of the PCR products obtained (Figure 8B). The calculation revealed a shift of the bcl-Xl/bax-α ratio from 0.4 in control PMNs to 3.1 inCD18−/− PMNs, which corresponds to a 7.8-fold increase of the ratio compared with control. This suggests that the profound shift of balance between these factors toward the antiapoptotic gene product may be involved in the observed delay of apoptosis inCD18−/− PMNs. To prove whether this shift of balance may be sufficient to delay apoptosis, we used the antisense technique using bax-α antisense oligonucleotides and scrambled oligonucleotides. As assessed by flow cytometry after intracellular immunofluorescence staining of Bax-α in permeabilized PMNs, we found a substantial down-regulation of Bax-α after antisense treatment when compared with the effect of the scrambled oligonucleotides (Figure 8C). This down-regulation of Bax-α, which mimicked the shift of balance observed inCD18−/− PMNs, was sufficient to prolong the lifetime of PMNs (Figure 8D). The analysis revealed that 17.2% of the cells survived within 24 hours after antisense treatment. In contrast, only 10.8% of the cells were nonapoptotic in the presence of scrambled antisense oligonucleotides. Thus, the survival rate was 1.6-fold increased in the presence of the antisense oligonucleotides demonstrating that a decrease of bax-α expression promotes PMN survival by delaying apoptosis. This shows that the observed shift of the balance observed in PMNs fromCD18−/− mice is sufficient to impair PMN apoptosis.
Decreased bax-α expression caused the delay of PMN apoptosis.
(A) Differential expression of bcl-Xl and bax-α in 4 different PMN samples (1-4) freshly isolated from the circulation ofCD18+/+ mice orCD18−/−, respectively, as measured by semiquantitative RT-PCR. (B) Alteration of the bcl-Xl/bax-α ratio on apoptosis as calculated from the mean optical density of the PCR products obtained from PMNs of 7 animals of each group. Numbers indicate the mean ratios ± SDs; **P < .005. (C) Flow cytometric analysis of the down-regulation of Bax-α in the presence of antisense oligonucleotides (bax-α-as) when compared with the effect of scrambled oligonucleotides (bax-α-sc). (D) Survival of wild-type PMNs in the presence of bax-α antisense (bax-α-as) or scrambled (bax-α-sc) oligonucleotides. Data represent means ± SDs; **P < .005; n = 10.
Decreased bax-α expression caused the delay of PMN apoptosis.
(A) Differential expression of bcl-Xl and bax-α in 4 different PMN samples (1-4) freshly isolated from the circulation ofCD18+/+ mice orCD18−/−, respectively, as measured by semiquantitative RT-PCR. (B) Alteration of the bcl-Xl/bax-α ratio on apoptosis as calculated from the mean optical density of the PCR products obtained from PMNs of 7 animals of each group. Numbers indicate the mean ratios ± SDs; **P < .005. (C) Flow cytometric analysis of the down-regulation of Bax-α in the presence of antisense oligonucleotides (bax-α-as) when compared with the effect of scrambled oligonucleotides (bax-α-sc). (D) Survival of wild-type PMNs in the presence of bax-α antisense (bax-α-as) or scrambled (bax-α-sc) oligonucleotides. Data represent means ± SDs; **P < .005; n = 10.
Finally, we addressed the question whether the observed delay of apoptosis is a primary effect that is directly caused by the absence of CD18 and measured PMN apoptosis inCD18+/+/CD18−/−chimeric mice. First of all, we analyzed the peripheral PMN counts of these animals and found a mild leukocytosis in these animals (Figure9A), which was due to the elevation of the lymphocyte counts (Figure 9B). In contrast, no difference in the peripheral PMN or monocyte counts was detectable when compared with the wild type. To study apoptosis of PMNs derived from theCD18+/+/CD18−/−chimeric mice, PMNs were isolated from the peripheral blood of these animals and CD18−/−and CD18+/+ PMNs were separated. Subsequently, cells were subjected to the analysis of the intracellular DNA content (Figure 10A). No difference of apoptosis was detectable between theCD18−/− and theCD18+/+ PMNs. A similar result was obtained when PMN apoptosis was measured in whole blood samples by detecting the diminished cell surface expression of CD16 (Figure 10B). After double staining with a FITC-labeled anti-CD16 mAb and a PE-labeled anti-CD18 mAb, no significant difference of apoptosis between the CD18−/− andCD18+/+ PMNs in the peripheral blood ofCD18+/+/CD18−/−chimeric mice was detectable. Thus, the presence of wild-type leukocytes abolished the delay of apoptosis inCD18−/− PMNs of the chimeric animals, suggesting that the observed delay of PMN apoptosis inCD18−/− mice is not simply a cellular effect.
Peripheral blood leukocyte counts inCD18+/+/CD18−/−chimeric mice.
Total (A) and differential leukocyte counts (B) in whole blood samples obtained fromCD18+/+/CD18−/−chimeric mice (n = 10) or wild-type control animals (n = 10). Data represent means ± SDs; **P < .01; NS indicates not significant.
Peripheral blood leukocyte counts inCD18+/+/CD18−/−chimeric mice.
Total (A) and differential leukocyte counts (B) in whole blood samples obtained fromCD18+/+/CD18−/−chimeric mice (n = 10) or wild-type control animals (n = 10). Data represent means ± SDs; **P < .01; NS indicates not significant.
Apoptosis ofCD18+/+ andCD18−/− PMNs derived fromCD18+/+/CD18−/−chimeric mice.
(A) Flow cytometric analysis of DNA content measured in PI-stainedCD18+/+ andCD18−/− PMNs isolated from the circulation ofCD18+/+/CD18−/−chimeric mice and aged for 4 hours in culture without further stimulation (n = 3). Data represent apoptotic PMNs with a loss of DNA content in percent of total cell number. Data represent means ± SDs; NS indicates not significant. (B) Flow cytometric analysis of CD16 expression on the cell surface ofCD18+/+ andCD18−/− PMNs in whole blood samples obtained from the circulation ofCD18+/+/CD18−/−chimeric mice and aged for 0 and 4 hours in culture without further stimulation using the FITC-labeled anti-CD16 mAb and the PE-labeled anti-CD18 mAb. Data represent apoptotic PMNs with diminished CD16 expression in percent of total cell number. Means ± SDs are shown; NS indicates not significant.
Apoptosis ofCD18+/+ andCD18−/− PMNs derived fromCD18+/+/CD18−/−chimeric mice.
(A) Flow cytometric analysis of DNA content measured in PI-stainedCD18+/+ andCD18−/− PMNs isolated from the circulation ofCD18+/+/CD18−/−chimeric mice and aged for 4 hours in culture without further stimulation (n = 3). Data represent apoptotic PMNs with a loss of DNA content in percent of total cell number. Data represent means ± SDs; NS indicates not significant. (B) Flow cytometric analysis of CD16 expression on the cell surface ofCD18+/+ andCD18−/− PMNs in whole blood samples obtained from the circulation ofCD18+/+/CD18−/−chimeric mice and aged for 0 and 4 hours in culture without further stimulation using the FITC-labeled anti-CD16 mAb and the PE-labeled anti-CD18 mAb. Data represent apoptotic PMNs with diminished CD16 expression in percent of total cell number. Means ± SDs are shown; NS indicates not significant.
Discussion
A recent report presented evidence that apoptosis is critical for the clearance of PMNs from the peripheral blood by Kupffer cells in the liver.20 In the present study, we analyzed the lifetime of circulating PMNs by measuring apoptosis. Using 4 independent methods, specifically, loss of DNA content, down-regulation of CD16 expression on the cell surface as well as analysis of nuclear morphology and DNA degradation, we were able to demonstrate that PMNs in the circulation of CD18−/− mice showed a profound impairment of apoptosis when compared with PMNs from wild-type control animals. Thus, our data support the concept that a delay of apoptosis contributes to the observed elevation of blood PMN counts in the circulation of CD18−/−mice. This in agreement with a previous study demonstrating that delayed PMN apoptosis in inflammation in humans leads to an expansion of the circulating PMN pool.7 In contrast to this study, we investigated apoptosis in a noninflammatory model. By means of extended microbiologic screening as well as by antibiotic treatment, it was ruled out that the animals used had severe infections. This may suggest that the control of apoptosis represents a mechanism that underlies the control of PMN homeostasis also in the absence of an inflammatory stimulus. In the study by Dibbert et al, the observed neutrophilia in inflammation was reported to be caused by elevated levels of the cytokines GM-CSF and G-CSF.7 In contrast, no increase of the GM-CSF concentration was observed in the plasma ofCD18−/− mice in our study. This suggests that GM-CSF is probably not sufficient for the observed delay of apoptosis in our model. This is true for IL-6, because the observed neutrophilia and the delay of apoptosis was also present inCD18−/−/IL-6−/−mice. However, the G-CSF concentration has been reported to be elevated in CD18−/−mice,21 but neutralizing G-CSF in the plasma ofCD18−/− mice did not alter the response of PMNs with respect to their susceptibility to undergo apoptosis. Moreover, plasma ofCD18−/− mice did not reduce apoptosis of wild-type PMNs, and plasma ofCD18+/+ mice was not able to accelerate apoptosis of PMNs derived from the circulation ofCD18−/− mice. Although IL-6 and G-CSF, for example, have been shown to delay PMN apoptosis,5 19 our data suggest that soluble mediators in the plasma alone are not sufficient to induce the observed delay of PMN apoptosis in theCD18−/− mice.
The β2 integrins mediate the firm adhesion of PMNs to the endothelial cells, which represents a prerequisite for PMN extravasation,17,22 and previous studies have shown that β2 integrins are involved in the control of the lifetime of emigrating PMNs by triggering apoptosis.23,24 Because apoptosis of CD18−/− PMNs obtained fromCD18+/+/CD18−/−chimeric mice was not delayed when compared with apoptosis ofCD18+/+ PMNs derived from the same animals, the present study suggests that the lack of β2 integrins on PMNs alone is not sufficient to cause the delay of apoptosis of circulating PMNs in vivo. The peripheral PMN pool consists of 2 fractions, that is, circulating PMNs and marginated PMNs that transiently interact with the blood vessels, especially in the capillary beds in the microcirculation of the lungs.25Although, the exact physiologic relevance of this phenomenon is not entirely clear, it may be possible that endothelial-derived paracrine signals in the vascular beds may contribute to the control of PMN apoptosis, which would explain that plasma failed to affect PMN apoptosis. Interestingly, bone marrow PMNs derived fromCD18−/− mice showed normal apoptosis when compared with PMNs from control animals, suggesting that the impairment of apoptosis is induced not before the PMNs reach the circulation. This may promote the idea that the delay of PMN apoptosis in the CD18−/− mice may be due to endothelial-derived paracrine signals that may be recognized by the PMNs during transient PMN-endothelial cell contacts. However, further investigations are necessary to clearly identify the mechanism by which the systemic absence of β2 integrins affects PMN apoptosis.
A recent report presented evidence that neutrophilia in the absence of CD18 was still present when the hematopoietic system of wild-type animals was replaced by CD18-deficient fetal liver cells, demonstrating that the absence of CD18 in the hematopoietic system alone is sufficient to cause an alteration of PMN homeostasis.26However, neutrophilia was almost resolved when the hematopoietic system of wild-type animals was replaced by a mixture of wild-type and CD18-deficient fetal liver cells. Using a similar model, increased granulopoiesis mediated by IL-17 and G-CSF21 has been reported in CD18−/− mice. Thus, both mechanisms, the control of granulopoiesis in the bone marrow as well as the control of PMN apoptosis in the circulation, may contribute to the control of PMN homeostasis.
We have previously shown that bcl-Xl and bax-α, members of the bcl-2 family of apoptosis-associated genes, play a pivotal role in the control of apoptosis of human PMNs in vitro.4 Now we present evidence that these genes are also involved in the control of PMN apoptosis in vivo. By means of a semiquantitative RT-PCR technique, we were able to demonstrate a marked up-regulation of the antiapoptotic gene product bcl-Xl and a profound down-regulation of the proapoptotic gene product bax-α. The bcl-2 family is known to regulate apoptosis by the control of the release of cytochrome c from mitochondria allowing the activation of caspases that finally execute the apoptotic program.27Using an antisense technique, we down-regulated bax-α and thereby mimicked one part of the observed shift of balance between proapoptotic and antiapoptotic members of the bcl-2 family. We found that this was sufficient to prolong PMN survival by a delay of apoptosis. However, in blood PMNs from CD18−/−mice, not only was bax-α found to be down-regulated but also bcl-Xl was up-regulated. Thus, the shift of the balance between the members of the bcl-2 family was even more pronounced in the situation in vivo, which may explain the fact that the observed delay of apoptosis was more profound inCD18−/− PMNs when compared with bax-α antisense-treated wild-type PMNs. Moreover, expression of A1, Bad, and Bak was not altered in PMNs fromCD18−/− mice when compared with wild-type control. Together, the data suggest that the observed delay of apoptosis is due to a differential regulation of bcl-Xl and bax-α, a finding that is in accordance with the study in which the delay of PMN apoptosis in inflammation in humans was found to be due to a down-regulation of bax-α.7 This may show that PMN apoptosis is mediated by differential expression of the bcl-2 family of apoptosis-associated genes not only in inflammation but also in the absence of an inflammatory stimulus, suggesting that this mechanism represents a general principle controlling the life span of PMNs in vivo. Altogether, the present study shows that not only proliferation, maturation, and release of PMNs from the bone marrow but also the control of PMN apoptosis in the circulation contribute to PMN homeostasis in the circulation under noninflammatory conditions. The intracellular mechanism that determines the lifetime of PMNs critically involves the differential expression of the bcl-2 family members bax-α and bcl-Xl, which control the apoptotic machinery of PMNs in vivo.
The expert technical assistance of Ms A. Günther and Ms R. Noske-Reimers is acknowledged.
Prepublished online as Blood First Edition Paper, September 12, 2002; DOI 10.1182/blood-2002-01-0239.
Supported by Deutsche Forschungsgemeinschaft (SFB 366/C3).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Barbara Walzog, Ludwig-Maximilians-Universität, Department of Physiology, Schillerstr 44, D-80336 München, Germany; e-mail:walzog@lrz.uni-muenchen.de.









This feature is available to Subscribers Only
Sign In or Create an Account Close Modal