To the Editor:
Two herpesviruses, human herpesvirus-8 (HHV-8) and Epstein-Barr virus (EBV), are able to contribute to lymphomagenesis in humans.1 HHV-8 is documented not only in a strong association with Kaposi’s sarcoma, but also in a high percentage of primary effusion lymphoma, Castleman’s disease, and multiple myeloma. Most recently, HHV-8 genome has been associated with primary central nervous system lymphoma (PCNSL) of patients with and without acquired immunodeficiency syndrome (AIDS).2 However, the role of HHV-8 in the pathogenesis of PCNSL remains controversial.3In vitro, EBV efficiently transforms human B lymphocytes, causing them to proliferate continuously.1 EBV and the latent membrane protein can be detected in tumor cells of almost all AIDS-related PCNSL.
Primary intraocular lymphoma, a component of PCNSL, is a large B-cell, non-Hodgkin’s lymphoma.4 The disease is aggressive, with a 5-year survival rate of less than 33%. In the past 15 years, the incidence of the tumor has increased dramatically, coincident with the AIDS epidemic. We analyzed HHV-8 and EBV DNA sequences in 13 primary intraocular lymphomas with and without AIDS. Of the 13 specimens, 5 were whole eyes, 1 was a vitreoretinal biopsy, and 7 were vitrectomy samples. Slides with cells from 2 noninfectious uveitis were also used as control.
The 13 patients (6 Americans and 7 Europeans) include 2 AIDS patients (1 American and 1 French patient): the American patient developed an early lymphoma and the French patient had an advanced stage, aggressive lymphoma.5 At the time at which the 13 specimens were obtained, only 3 (2 eyes and 1 vitrectomy specimen) had a proven diagnosis of PCNSL involving the eyes. Of the 5 eyes, 2 had received radiation therapy. Nine patients were being investigated for possible primary intraocular lymphoma and underwent diagnostic procedures (7 vitrectomies, 1 vitreoretinal biopsy, and 1 enucleation). The eye of the American AIDS patient was diagnosed with primary intraocular lymphoma at necropsy.
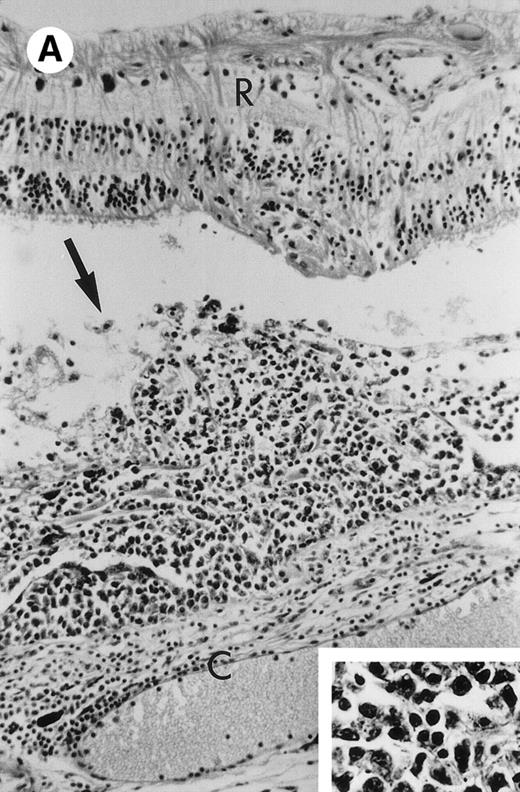
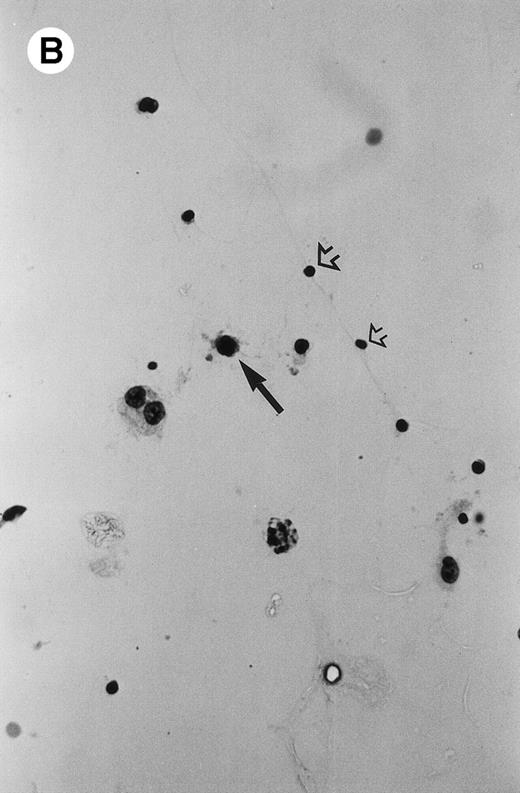
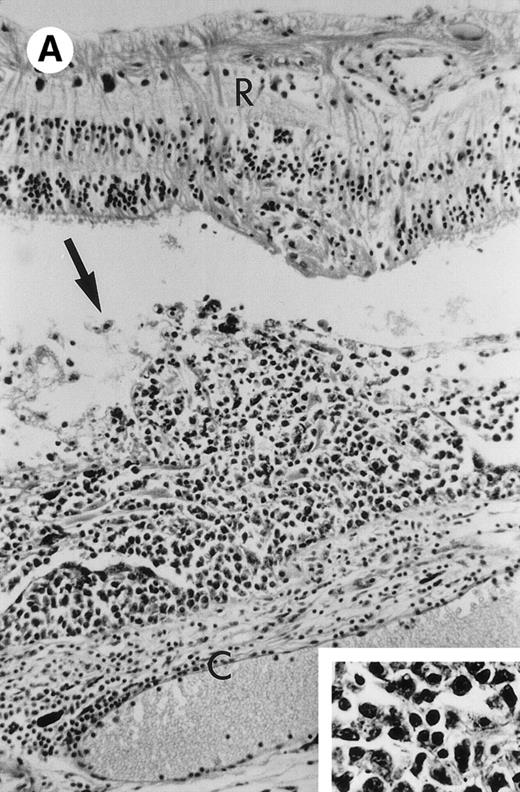
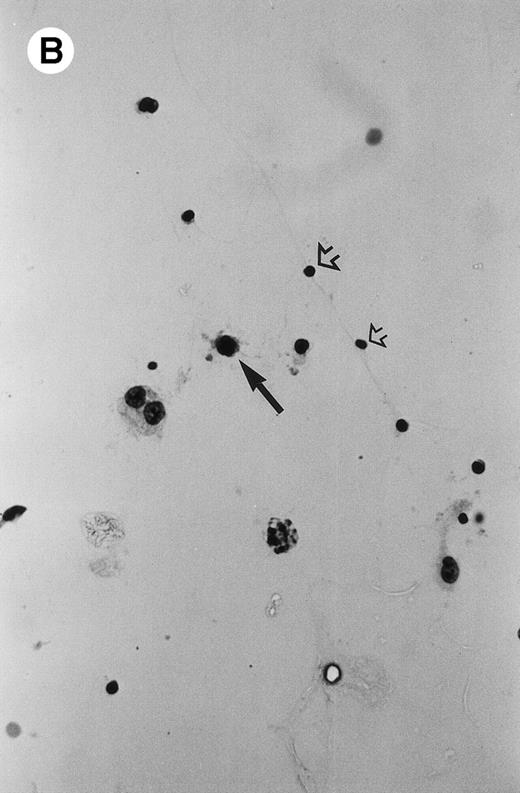
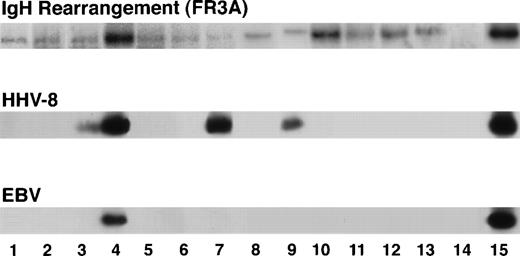
On examination of the histology and cytology slides of the 13 cases, only 6 specimens (3 of 5 eyes, 3 of 7 vitrectomies, and 0 of 1 vitreoretinal biopsy) showed typical large B-cell lymphoma (Fig1). Of the 7 cases without obvious typical lymphoma cells, 5 (4 vitreous and 1 vitreoretinal biopsy) were also available for cytokine analysis and had high vitreous interleukin-10 (IL-10) levels with high ratios of IL-10 to IL-6, suggesting primary intraocular lymphoma.6Finally, 2 cases (1 eye with AIDS and 1 eye that had received radiation) showed only a few atypical lymphocytes in the subretinal space. The microdissected morphologically suspicious abnormal cells in all 13 cases had presented a rearrangement in FR3A of the IgH gene that confirmed the diagnosis of primary intraocular lymphoma (Fig 2).5
Microphotograph showing typical intraocular lymphoma (arrow) in the subretinal space (A; case no. 8; insert, higher magnification of the lymphoma cells; R, retina; C, choroid) and a vitrectomy specimen (B; case no. 7; arrowheads, normal lymphocytes). (Original magnifications: A, hematoxylin & eosin, ×200, insert, ×400; B, Diff-Quick, ×400.)
Microphotograph showing typical intraocular lymphoma (arrow) in the subretinal space (A; case no. 8; insert, higher magnification of the lymphoma cells; R, retina; C, choroid) and a vitrectomy specimen (B; case no. 7; arrowheads, normal lymphocytes). (Original magnifications: A, hematoxylin & eosin, ×200, insert, ×400; B, Diff-Quick, ×400.)
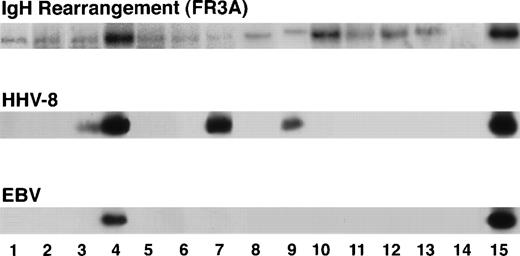
PCR amplification showing rearrangement of third framework region in the VH region of heavy chain Ig gene in the lymphoma cells of all 13 cases, HHV-8 genome in 4 cases (lanes 3 and 4, AIDS patients; lanes 7 and 9, non-AIDS patients), and EBV genome in 1 case (lane 4, AIDS with lymphoma involving the orbit and eye). Lanes 1 through 13, cases no. 1 through 13, respectively; lane 14, negative control; lane 15, positive control.
PCR amplification showing rearrangement of third framework region in the VH region of heavy chain Ig gene in the lymphoma cells of all 13 cases, HHV-8 genome in 4 cases (lanes 3 and 4, AIDS patients; lanes 7 and 9, non-AIDS patients), and EBV genome in 1 case (lane 4, AIDS with lymphoma involving the orbit and eye). Lanes 1 through 13, cases no. 1 through 13, respectively; lane 14, negative control; lane 15, positive control.
Lymphoma cells of these 13 specimens, normal lymphocytes of 2 vitrectomy specimens, and the 2 uveitic cases were microdissected from either deparaffinized sections or cytological slides.5 DNA of these cells were extracted for polymerase chain reaction (PCR) amplification and Southern hybridization for HHV-8 or EBV genome. Multiple primers and positive and negative controls were also used to confirm the results.
Four cases were positive for HHV-8 (Fig 2). Two were the AIDS-related lymphoma eyes and 2 were non-AIDS vitreous samples. The 2 non-AIDS patients were diagnosed with suspicious primary intraocular lymphoma both clinically and cytopathologically. These 4 positive patients included 2 Americans and 2 French. Three samples (1 American AIDS eye and 2 vitreous specimens) were also microdissected to obtain nonmalignant cells (retinal and optic nerve cells from the eye and infiltrating lymphocytes from the other 2 vitreous specimens) for identification of the viral genome. HHV-8 DNA was undetectable in the inflammatory or ocular cells without tumor infiltration in the 3 early cases with primary intraocular lymphoma. EBV DNA was detected in only 1 of the 13 samples, ie, the French AIDS eye with a diffuse lymphoma.
This investigation has shown HHV-8 DNA sequences in 2 of 2 AIDS-related intraocular lymphoma and in 2 of 11 non-AIDS intraocular lymphoma. The HHV-8 genome encodes homologs of cyclin D1, a cell-cycle control element; certain cytokines, regulators, and receptors; and Bcl-2, an antiapoptotic protein.7 The HHV-8 sequence also contains homologs of vial IRFs that may be involved in modulating both HHV-8 replication and HHV-8–associated tumorigenicity.8 The viral genome could therefore contribute to cellular growth and transformation through activation of the cell cycle. Although the virus could simply be an innocent passenger in this lymphoma, the so-far ubiquitous association of HHV-8 with AIDS-related PCNSL and relatively low incidence in non-AIDS patients, plus most other lymphoproliferative disorders in both AIDS and non-AIDS patients, strongly favor a causal role. In this series, HHV-8 was detected in 100% (2 cases: 1 American and 1 French) of AIDS-related intraocular lymphoma and in 1 of the 6 European and 1 of the 5 American, non-AIDS cases. Furthermore, HHV-8 DNA was found only in the neoplastic cells. We speculate that the nonneoplastic B lymphocytes in those AIDS patients who eventually develop primary intraocular lymphoma may be infected with HHV-8, HIV, or other viruses into the eye, in which ultimate transformation into malignant cells occurs. Another possibility may be the promotion of a second oncogenic virus.
Nine EBV genes are known to express as proteins in EBV-transformed B-lymphoblastoid cell lines.9 One of the latent membrane proteins of the EBV engages members of the tumor necrosis factor receptor-associated molecules and then activates NF-κB–driven expression of multiple viral and cellular genes. However, only certain subsets of AIDS-non Hodgkin’s lymphoma appear to be EBV-related, although a high frequency of EBV is reported in AIDS-PCNSL.10 Our data do not show a strong association between EBV and primary intraocular lymphoma, suggesting that EBV may not play a major role in the early development of primary intraocular lymphoma with or without AIDS.