Abstract
Adenoviruses are efficient gene delivery agents for a variety of neoplasms. In the present study, we have investigated the use of adenoviruses for the delivery of the thymidine kinase(tk) gene into multiple myeloma (MM) cells. We first demonstrated that MM cell lines and MM patient cells express both adenovirus receptors as well as the DF3/MUC1 protein, thus providing a rationale for using adenoviruses to selectively deliver genes under the control of the DF3 promoter. By using an adenoviral construct containing β-galactosidase (β-gal) gene driven by the DF3 promoter (Ad.DF3-βgal), we demonstrate greater than 80% transduction efficiency in OCI-My5 and RPMI 8226 MM cell lines at a multiplicity of infection of 1 to 100. Importantly, transduction with the tk gene driven by the DF3 promoter (Ad.DF3-tk)followed by treatment with 50 μmol/L ganciclovir (GCV) purged ≥6 log of contaminating OCI-My5 and RPMI 8226 MM cells within bone marrow mononuclear cells. In contrast, normal human hematopoietic progenitor cell number was unaffected under these conditions. Selectivity of DF3/MUC1 promoter was further confirmed, because Ad.DF3-βgalor Ad.DF3-tk did not transduce MUC1-negative HeLa cervical carcinoma cells. In addition, GCV treatment of Ad.DF3-tk–transduced RPMI 8226 MM cells did not induce a significant bystander effect. These findings demonstrate that transduction with Ad vectors using a tumor-selective promoter provides a highly efficient and selective approach for the ex vivo purging of MM cells.
HIGH-DOSE CHEMORADIOTHERAPY followed by transplantation of either autologous bone marrow (BM) or peripheral blood progenitor cells (PBPCs) has achieved high (40%) complete response (CR) rates in patients with multiple myeloma (MM), but the median duration of these responses has unfortunately been only 24 to 36 months at best.1,2 Patients with sensitive disease and who are less heavily pretreated have the most favorable outcomes. Most importantly, a national French trial of 200 patients with MM has demonstrated significantly higher response, event-free survival (EFS), and overall survival (OS) rates for those patients treated with high-dose treatment, compared with those receiving conventional therapy.3 This study is encouraging and additional randomized trials in the United States, Scandinavia, Spain, and England are also comparing the outcome of conventional therapy versus high-dose therapy and autografting. However, it is unlikely that any patients with MM are cured after a single high-dose therapy and stem cell autografting regimen.
Attempts to improve on the outcome of high-dose therapy followed by autografting are directed, first, to improve response rates and achieve minimal residual disease (MRD) with transplant and, second, to develop strategies for the treatment of MRD posttransplant to achieve prolonged disease-free survival (DFS) and potential cure. One example of an attempt to improve outcome after autografting is the use of multiple high-dose therapies followed by stem cell transplantation. Outcome appears superior to historically matched controls treated with conventional therapy,4,5 and the relative efficacy of a single versus double transplant is being evaluated in a randomized trial.6 Giralt et al7 have recently reported on the use of cyclosporine to induce graft-versus-host disease (GVHD) post autografting in an attempt to generate the associated graft-versus-myeloma effect (GVM) and achieve the second goal, namely to effectively treat MRD posttransplant.
Mutiple efforts have also been undertaken to obtain tumor-free BM or PBPC autografts for transplantation. These include depletion of MM cells from autografts,8-10 selection of normal hematopoietic progenitor cells (HPCs) within autografts by virtue of CD34+ expression,11,12 and selection of normal HPCs using multiparameter cell sorting.13 Monoclonal antibody (MoAb)-purged BM transplantation can achieve depletion of 2 to 3 log of tumor cells from autografts but few, if any, long-term disease-free survivors.1,8-10 Although up to 5 log depletion of MM cells can be achieved using CD34+ selection of PBPCs, nearly half of CD34+ autografts still contain residual tumor cells and the clinical impact of CD34+selection requires further follow-up.11,12,14-16 A promising highly efficient depletion of tumor cells from autografts can be achieved by transducing PBPCs ex vivo using a vector expressing the herpes simplex virus (HSV) thymidine kinase (tk) gene, followed by treatment with ganciclovir (GCV). For example, we have previously used replication-defective recombinant adenoviral vectors (Ad) containing the cytomegalovirus (CMV) or DF3/MUC1 promoters to selectively transduce contaminating breast carcinoma cells within autografts with tk gene; subsequent GCV treatment eliminated 6 log of contaminating breast cancer cells.17
In the present study, we demonstrate that MM cell lines and freshly isolated patient MM cells, but not normal BM mononuclear cells (MNCs), express adenovirus receptors. Moreover, these MM cells also express DF3/MUC1, suggesting that selectivity of transgene expression may be achieved using adenoviral vectors under the control of the DF3/MUC1 promoter. By using an adenoviral construct containingβ-galactosidase (β-gal) gene driven by the DF3 promoter (Ad.DF3-βgal), we demonstrate greater than 80% transduction efficiency of OCI-My5 and RPMI 8226 MM cells at a multiplicity of infection (MOI) of 1 to 100. Importantly, transduction with the tk gene driven by the DF3 promoter (Ad.DF3-tk) followed by treatment with 50 μmol/L GCV purged ≥6 log of contaminating OCI-My5 and RPMI 8226 MM cells within BM MNCs, without adversely affecting normal HPCs. Furthermore, GCV treatment of AD.DF3-tk–transduced MM cells did not induce a bystander effect. Our data therefore indicate that Ad.DF3-tk may provide a highly efficient and selective approach for the ex vivo purging of MM cells.
MATERIALS AND METHODS
Cell lines and transfectants.
The following cell lines were obtained from American Type Culture Collection (ATCC; Rockville, MD): RPMI 8226 (CCL-155), ARH-77 (CRL-1621), HS Sultan (CRL-1484), and IM-9 (CCL-159) MM cell lines; CESS (TIB-190) Epstein-Barr virus (EBV)-transformed B cells; HeLa (CCL-2) cervical carcinoma cells; and RD rhabdomyosarcoma (CCL-136) cells. OCI-My5 MM cells were kindly provided by Dr H.A. Messner (Ontario Cancer Institute, Toronto, Ontario, Canada); and JY EBV-transformed B cells by Dr J.D. Fingeroth (Dana-Farber Cancer Institute, Boston, MA). RD CAR, RD rhabdomyosarcoma cells transfected with CAR adenovirus receptor cDNA, and RD PCR3, RD cells transfected with the PCR3 plasmid vector alone that contains the neomycin resistance (NeoR) gene, were produced by lipofectamine-mediated gene transfer (GIBCO BRL, Gaithersburg, MD) and selected with media containing 1 mg/mL of neomycin. Patient MM1 and MM2 cells (>99% CD38+CD45RA−), normal B splenocytes from a cadaveric donor (T-cell and monocyte depleted), and BM MNCs from normal donors were obtained by Ficoll-Paque (Pharmacia Biotech, Uppsala, Sweden) density gradient separation after informed consent had been obtained.
RPMI 8226, ARH-77, HS Sultan, and IM-9 MM cells; patient MM1 and MM2 cells; normal B splenocytes; CESS and JY EBV-transformed B cells; and normal BM MNCs were cultured in 90% RPMI-1640 with L-glutamine medium supplemented with 25 IU/mL penicillin, 25 μg/mL streptomycin, 5 mmol/L L-glutamine (all from GIBCO BRL), and 10% fetal bovine serum (FBS; Sigma Diagnostics, St Louis, MO). OCI-My5 MM cells and BM MNCs were cultured in 90% Iscove’s modified Dulbecco’s medium (Sigma Diagnostics), 10% FBS, 25 IU/mL penicillin, 25 μg/mL streptomycin, and 5 mmol/L L-glutamine. HeLa cells were maintained in 90% Dulbecco’s modified Eagle’s medium (DMEM) with 4,500 mg/L D-glucose (GIBCO BRL), 10% FBS, 1 mmol/L MEM sodium pyruvate (GIBCO BRL), 25 IU/mL penicillin, 25 μg/mL streptomycin, and 5 mmol/L L-glutamine. RD cells were cultured in 90% Eagle’s minimum essential medium with nonessential amino acids and Earle’s balanced salt solution (GIBCO BRL), 10% FBS, 25 IU/mL penicillin, 25 μg/mL streptomycin, and 5 mmol/L L-glutamine. All cells were cultured at 37°C in a humidified 5% CO2 atmosphere. BM MNCs were treated with 2.0 Gy of γ-irradiation before tumor cell contamination and purging assays.
Antibodies for indirect immunofluorescence flow cytometry.
The following antibodies were used in indirect immunofluorescence flow cytometry: RmcB anti-CAR adenovirus receptor mouse MoAb,18B5-IA9 anti-αvβ5 integrin MoAb (generously provided by Dr Martin E. Hemler, Dana-Farber Cancer Institute),19 DF3 anti-MUC1 MoAb,20 fluorescein isothiocyanate (FITC)-conjugated goat (Fab′)2 antimouse IgG MoAb (Immunotech, Westbrook, ME), and FITC-conjugated mouse IgG1 (Coulter Corp, Miami, FL). Flow cytometric analysis was performed using the Coulter Epics XL flow cytometer (Coulter Corp).
Specific 35S-Ad2 binding assays.
To confirm specific Ad2 binding, a competitive MoAb blocking assay was performed by preincubating OCI-My5, RPMI 8226, ARH-77, HS Sultan, and IM-9 MM cells; patient MM1 cells; normal B splenocytes; CESS and JY EBV-transformed B cells; normal BM MNCs; HeLa cells (known to express CAR protein); RD CAR cells (positive control); and RD PCR3 (negative control) cells (1 × 106) with RmcB anti-CAR blocking MoAb (1:100 dilution) at 4°C for 1 hour. Similarly, preincubation with 5E2B4 mouse MoAb (IgG2; 1:100 dilution), which targets a nonsurface protein, was used as an isotype control. Cells were next incubated in triplicate with 20,000 cpm of 35S-Ad2 radiolabeled adenovirus18 in 200 μL of Hank’s Balanced Salt Solution (HBSS; GIBCO BRL) at room temperature for 1 hour. Excess MoAb was then washed off thrice with HBSS and cells were solubilized in 500 μL of SOLVABLE (DuPont NEN, Boston, MA). Ten milliliters of Formula 989 (DuPont NEN) was added, and 35S-Ad2 binding was analyzed on the LS 6000SC beta-scintillation counter (Beckman Instruments, Inc, Fullerton, CA).
Adenovirus transduction.
Ad.DF3-βgal and Ad.DF3-tk are Ad vectors in which theβ-gal and tk genes, respectively, are under control of the DF3/MUC1 tumor-selective promoter.21-23Ad.CMV-βgal and Ad.CMV-tk are vectors in which the same genes are under control of the CMV immediate-early promoter and enhancer24 (kindly provided by Dr Robert Gerard, University of Texas, Austin, TX). Cells were transduced with adenovirus at MOI of 1 to 100 for 2 hours, washed out for 10 hours, resuspended in fresh media, and evaluated for the expression of the transgene at 24 to 48 hours after transduction.
β-Galalactosidase activity assays.
Expression of the transgene was assessed by β-gal activity using fluorescence-activated flow cytometry, as previously described.25 Briefly, 0.5 to 1.0 × 106cells were suspended in 50 μL of serum-free culture media at 37°C. An equal volume of 2 mmol/L fluorescein di-β-D-galactopyranoside (FDG; Molecular Probes, Eugene, OR) was added, rapidly mixed, and incubated at 37°C for 1 minute. The cells were next washed once with 4 mL of ice-cold phosphate-buffered saline (PBS) and maintained in ice-cold PBS until analysis. The β-gal activity of transduced cells was also determined using a chemiluminescence assay (Galacto-Light system; Tropix, Inc, Bedford, MA) that detects 2 fg to 20 ng of β-galactosidase26 and by 5-bromo-4-chloro-3-indolyl-β-D-galactoside (X-Gal; GIBCO BRL) staining. For X-Gal staining, tumor cells were washed three times in PBS; fixed in 0.5% glutaldehyde; washed a further three times with PBS/2 mmol/L MgCl2; stained at 37°C overnight with 2 mg/mL X-Gal, 5 mmol/L K3Fe(CN)6 and 5 mmol/L K4 Fe(CN)6·3H2O in PBS/2 mmol/L MgCl2; and counted by light microscopy (200 cells/sample; n = 3).
Cell proliferation assay.
MM cell line proliferation assays were used to define residual viable tumor cells remaining after treatment of Ad.DF3-tk– and Ad.CMV-tk–transduced MM cells within normal BM MNCs with varying concentrations (0 to 50 μmol/L) of GCV (CYTOVENE; Syntex Laboratories, Inc, Palo Alto, CA). After GCV treatment, transduced tumor cells alone or tumor cells mixed with γ-irradiated normal BM MNCs were incubated in triplicate in 96-well tissue culture plates with 1 μCi of tritiated thymidine (3H-TdR; DuPont NEN) for 12 hours, harvested onto glass filters using the HARVESTAR 96 MACH II harvester (Tomtec Inc, Orange, CT), and analyzed on the 1205 BETAPLATE beta-counter (Wallac, Gaithersburg, MD). Viable cell density was determined by trypan blue exclusion.
Human hematopoietic progenitor cell assays.
Colony-forming units–granulocyte-macrophage (CFU-GM) and burst-forming units-erythroid (BFU-E) were analyzed by plating BM MNCs (2 × 105 cells/well) obtained after Ficoll-Paque density gradient separation in Iscove’s methylcellulose medium (MethoCult GF H4434; Stem Cell Technologies, Vancouver, British Columbia, Canada) containing recombinant human stem cell factor (rhSCF; 50 ng/mL), recombinant human granulocyte-macrophage colony-stimulating factor (rhGM-CSF; 10 ng/mL), recombinant human interleukin-3 (rhIL-3; 10 ng/mL), and recombinant human erythropoietin (rhEPO; 3 U/mL).27 CFU-GM (≥40 cells) and BFU-E (≥3 erythroid clusters) colonies were enumerated and classified on the basis of morphology at 14 days of culture using indirect microscopy.
Polymerase chain reaction (PCR) detection of Ad5 E2B gene.
PCR of Ad5 E2B gene was used to detect transduced cells. Cells were washed three times in PBS, resuspended in 0.2 mL of TE buffer (10 mmol/L Tris pH 8.0, 1 mmol/L EDTA), lysed by freeze-thaw (×2), and centrifuged to remove cellular DNA and debris. The supernatant containing viral DNA was incubated with 100 mmol/L Tris, pH 8.0, 0.5% sodium dodecyl sulphate, and 200 μg/mL proteinase K (Sigma Diagnostics) at 50°C for 2 hours; and viral DNA was obtained by phenol/chloroform (GIBCO BRL) extraction followed by 100% ethanol/sodium acetate (Sigma Diagnostics) precipitation.28The E2B gene was amplified using the GeneAmp PCR reagent kit and Perkin-Elmer thermal cycler (Applied Biosystems Corp, Foster City, CA) under the following conditions: 94°C for 5 minutes, 94°C for 30 seconds (denaturation), 56°C for 30 seconds (annealing), and 72°C for 1 minute (extension) for 25 cycles; and 72°C for 10 minutes.17,28 The primers used for Ad5 E2B gene were 5′-TCGTTTCTCAGCAGCTGTTG-3′ (forward) and 5′-CATCTGAACTCAAAGCGTGG-3′ (reverse).28 β-actin (control) gene was amplified using the following primers: 5′-CAGCCATGTACGTTGCTATCCAG-3′ (forward) and 5′-GTTTCGTGGATGCCACAGGAC-3′ (reverse).
RESULTS
Expression of CAR adenovirus receptor on HeLa cells; OCI-My5, RPMI 8226, ARH-77, HS Sultan, and IM-9 MM cells; patient MM1 cells; normal B splenocytes; CESS and JY EBV-transformed B cells; and normal BM MNCs.
To explore the feasibility of using adenoviral vector transduction of MM cells with the tk gene followed by GCV treatment for purging MM cells, we first characterized the expression of adenoviral receptors on MM cells by indirect immunofluorescence flow cytometric analysis with RmcB anti-CAR adenoviral receptor MoAb (Fig 1).18 In this assay, RD PCR3 rhabdomyosarcoma cells transfected with vector alone served as a negative control (Fig 1A). RD rhabdomyosarcoma cells transduced withCAR adenovirus receptor gene (Fig 1B) and HeLa cells (Fig 1C), which are known to express adenoviral receptors, served as positive controls. Reactivity was observed on 5 MM cell lines (OCI-My5, RPMI 8226, ARH-77, HS Sultan, and IM-9; Fig 1D through H) and patient MM 1cells (Fig 1I) but absent on normal B splenocytes (Fig 1J), CESS and JY EBV-transformed B cells (Fig 1K and L), and normal BM MNCs (Fig 1M).
Expression of CAR adenovirus receptor on HeLa cells; OCI-My5, RPMI 8226, ARH-77, HS Sultan, and IM-9 MM cells; patient MM1 cells; normal B splenocytes; CESS and JY EBV-transformed B cells; and normal BM MNCs. Cells (5 × 105/mL) were stained with RmcB anti-CAR MoAb (1:100) followed by 1 μL of FITC-conjugated goat (Fab′)2 antimouse IgG MoAb, or with 5 μL of FITC-conjugated mouse IgG1 (isotype control), and analyzed by indirect immunofluorescence flow cytometry. Cells examined included RD PCR3 (A; negative control) and RD CAR (B; positive control) cells; HeLa (C) cells, known to express adenovirus receptors; OCI-My5 (D), RPMI 8226 (E), ARH-77 (F), HS Sultan (G), and IM-9 (H) MM cells; patient MM1 (I) cells; normal B splenocytes (J); CESS (K) and JY (L) EBV-transformed B cells; and normal BM MNCs (M).
Expression of CAR adenovirus receptor on HeLa cells; OCI-My5, RPMI 8226, ARH-77, HS Sultan, and IM-9 MM cells; patient MM1 cells; normal B splenocytes; CESS and JY EBV-transformed B cells; and normal BM MNCs. Cells (5 × 105/mL) were stained with RmcB anti-CAR MoAb (1:100) followed by 1 μL of FITC-conjugated goat (Fab′)2 antimouse IgG MoAb, or with 5 μL of FITC-conjugated mouse IgG1 (isotype control), and analyzed by indirect immunofluorescence flow cytometry. Cells examined included RD PCR3 (A; negative control) and RD CAR (B; positive control) cells; HeLa (C) cells, known to express adenovirus receptors; OCI-My5 (D), RPMI 8226 (E), ARH-77 (F), HS Sultan (G), and IM-9 (H) MM cells; patient MM1 (I) cells; normal B splenocytes (J); CESS (K) and JY (L) EBV-transformed B cells; and normal BM MNCs (M).
Specific 35S-Ad2 binding to HeLa cells; to OCI-My5, RPMI 8226, ARH-77, HS Sultan, and IM-9 MM cells; to patient MM1 cells; to normal B splenocytes; to CESS and JY EBV-transformed B cells; and to normal BM MNCs.
To confirm the presence of adenovirus receptors on MM cells and to compare the relative affinity of viral binding to MM cells versus cells of other lineages, we performed assays of specific 35S-Ad2 binding to tumor cells relative to HeLa cells (Fig 2). Preincubation of tumor cells with RmcB anti-CAR adenovirus receptor blocking MoAb defined the levels of nonspecific Ad2 binding; and preincubation with 5E2B4 mouse MoAb (IgG2) was used as an unreactive isotype control. RD CAR (184% specific HeLa binding) and RD PCR3 (0% specific HeLa binding) transfectants served as positive and negative controls for total Ad2 binding, respectively. MM cell lines (OCI-My5, RPMI 8226, ARH-77, HS Sultan, and IM-9) and patient MM1 cells demonstrated 25% to 100% specific adenoviral binding, compared with HeLa cells (100% specific Ad2 binding). In contrast, normal B splenocytes, CESS and JY EBV-transformed B cells, and normal BM MNCs did not exhibit significant binding of adenovirus.
Specific 35S-Ad2 binding to HeLa cells; to OCI-My5, RPMI 8226, ARH-77, HS Sultan, and IM-9 MM cells; to patient MM1 cells; to normal B splenocytes; to CESS and JY EBV-transformed B cells; and to normal BM MNCs. HeLa cells; OCI-My5, RPMI 8226, ARH-77, HS Sultan, and IM-9 MM cells; patient MM1 cells; normal B splenocytes; CESS and JY EBV-transformed B cells; and normal BM MNCs (1 × 106) were incubated with either RmcB anti-CAR MoAb (1:100) or 5E2B4 mouse MoAb (IgG2; 1:100; isotype control), followed by incubation with 35S-labeled Ad2, and then washed, solubilized, and analyzed on a β-counter. The percentage of specific Ad2 binding (difference in Ad2 binding by 5E2B4-treated versus RmcB-treated cells) relative to control HeLa cells (100% specific Ad2 binding) was determined. RD PCR3 and RD CAR transfectants served as negative and positive controls, respectively.
Specific 35S-Ad2 binding to HeLa cells; to OCI-My5, RPMI 8226, ARH-77, HS Sultan, and IM-9 MM cells; to patient MM1 cells; to normal B splenocytes; to CESS and JY EBV-transformed B cells; and to normal BM MNCs. HeLa cells; OCI-My5, RPMI 8226, ARH-77, HS Sultan, and IM-9 MM cells; patient MM1 cells; normal B splenocytes; CESS and JY EBV-transformed B cells; and normal BM MNCs (1 × 106) were incubated with either RmcB anti-CAR MoAb (1:100) or 5E2B4 mouse MoAb (IgG2; 1:100; isotype control), followed by incubation with 35S-labeled Ad2, and then washed, solubilized, and analyzed on a β-counter. The percentage of specific Ad2 binding (difference in Ad2 binding by 5E2B4-treated versus RmcB-treated cells) relative to control HeLa cells (100% specific Ad2 binding) was determined. RD PCR3 and RD CAR transfectants served as negative and positive controls, respectively.
Expression of αvβ5 integrin and DF3/MUC1 on OCI-My5 and RPMI 8226 MM cells as well as patient MM1 cells.
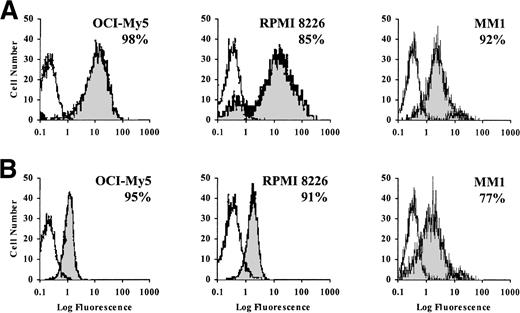
Because internalization of adenovirus into mammalian cells requires viral binding to αvβ5integrin29,30 and all β5 integrin subunits are associated with αv subunits,19 we assayed αvβ5 integrin expression on CAR adenovirus receptor-positive OCI-My5 and RPMI 8226 MM cells, as well as patient MM1 cells, using B5-IA9 anti-αvβ5MoAb19 in indirect immunofluorescence flow cytometry. Both MM cell lines and patient MM1 cells strongly expressed (85% to 98%) αvβ5 integrin (Fig 3A). Because prior reports have shown that MM cell lines and patient MM cells express DF3/MUC1,31 32 we examined our MM cell lines and patient MM1 cells for DF3/MUC1 expression (Fig 3B). Indirect immunofluorescence flow cytometric analysis confirmed strong (77% to 95%) DF3/MUC1 expression on MM cell lines and patient MM1 cells. Collectively, these findings suggest that DF3/MUC1 adenoviral vector-based therapies may offer the advantage of tumor cell selectivity.
Expression of vβ5 integrin and DF3/MUC1 on OCI-My5 and RPMI 8226 MM cells and on patient MM1 cells. OCI-My5 and RPMI 8226 MM cells and patient MM1 cells (5 × 105/mL) were stained with 1 μL of either vβ5 MoAb (A) or anti-DF3/MUC1 MoAb (B), followed by 1 μL of FITC-conjugated goat (Fab′)2antimouse IgG MoAb, or with 5 μL of FITC-conjugated mouse IgG1 alone (isotype control). The percentage of cells expressing these antigens was determined using indirect immunofluorescence flow cytometric analysis.
Expression of vβ5 integrin and DF3/MUC1 on OCI-My5 and RPMI 8226 MM cells and on patient MM1 cells. OCI-My5 and RPMI 8226 MM cells and patient MM1 cells (5 × 105/mL) were stained with 1 μL of either vβ5 MoAb (A) or anti-DF3/MUC1 MoAb (B), followed by 1 μL of FITC-conjugated goat (Fab′)2antimouse IgG MoAb, or with 5 μL of FITC-conjugated mouse IgG1 alone (isotype control). The percentage of cells expressing these antigens was determined using indirect immunofluorescence flow cytometric analysis.
Efficiency of Ad vector transduction assessed by β-gal reporter gene expression in OCI-My5 and RPMI 8226 MM cells as well as RPMI 8226 MM cells within normal BM MNCs.
We next determined the efficiency of adenovirus vector-mediated reporter gene expression in MM cells using Ad.DF3-βgal vector (Fig 4A). β-gal activity was observed in 80% to 100% of OCI-My5 and RPMI 8226 MM cells transduced with Ad.DF3-βgal at MOI = 1. To determine whether transduction using Ad vectors under the control of the DF3/MUC1 promoter may augment transduction efficiency for tumor cells, we compared the relative transduction efficiencies using Ad.CMV-βgal (nonspecific CMV promoter) or Ad.DF3-βgal (Fig 4B). Transduction efficiency, reflected in β-gal activity, was similar in OCI-My5 and RPMI 8226 MM cells using either promoter.
Efficiency of Ad vector transduction assessed byβ-gal reporter gene expression in OCI-My5 and RPMI 8226 MM cells, as well as RPMI 8226 MM cells within normal BM MNCs. OCI-My5 and RPMI 8226 MM cells (5 × 105/mL) were transduced with Ad.DF3-βgal at MOI = 1 for 2 hours, incubated with FDG, and analyzed by fluorescence flow cytometry at 24 hours (A). These tumor cells were also transduced with Ad.DF3-βgal (▪) or Ad.CMV-βgal (□) at MOI = 10 for 2 hours and analyzed by chemiluminescence assay at 24 hours (B). Mock-irradiated (□) and γ-irradiated (▪; 2.0 Gy) normal BM MNCs (3 × 104/well) were cultured in media alone or transduced with either Ad.CMV-βgal or Ad.DF3-βgal (both MOI = 100) for 2 hours and then analyzed by X-Gal staining at 24 hours (n = 3). X-Gal staining of mock-irradiated and γ-irradiated BM MNCs was compared with untransduced normal BM MNCs (negative control) and RPMI 8226 MM cells (positive control; C). RPMI 8226 MM cells (0.0%, 0.0001%, 0.001%, and 0.01%) mixed with normal BM MNCs were transduced with Ad.DF3-βgal at MOI = 1 for 2 hours and similarly analyzed using a chemiluminescence assay at 24 hours (n = 3; D).
Efficiency of Ad vector transduction assessed byβ-gal reporter gene expression in OCI-My5 and RPMI 8226 MM cells, as well as RPMI 8226 MM cells within normal BM MNCs. OCI-My5 and RPMI 8226 MM cells (5 × 105/mL) were transduced with Ad.DF3-βgal at MOI = 1 for 2 hours, incubated with FDG, and analyzed by fluorescence flow cytometry at 24 hours (A). These tumor cells were also transduced with Ad.DF3-βgal (▪) or Ad.CMV-βgal (□) at MOI = 10 for 2 hours and analyzed by chemiluminescence assay at 24 hours (B). Mock-irradiated (□) and γ-irradiated (▪; 2.0 Gy) normal BM MNCs (3 × 104/well) were cultured in media alone or transduced with either Ad.CMV-βgal or Ad.DF3-βgal (both MOI = 100) for 2 hours and then analyzed by X-Gal staining at 24 hours (n = 3). X-Gal staining of mock-irradiated and γ-irradiated BM MNCs was compared with untransduced normal BM MNCs (negative control) and RPMI 8226 MM cells (positive control; C). RPMI 8226 MM cells (0.0%, 0.0001%, 0.001%, and 0.01%) mixed with normal BM MNCs were transduced with Ad.DF3-βgal at MOI = 1 for 2 hours and similarly analyzed using a chemiluminescence assay at 24 hours (n = 3; D).
We next mixed Ad.DF3-βgal–transduced RPMI 8226 MM cells (0.01% to 0.0001%) within γ-irradiated normal BM MNCs to assess the level of detectability by chemiluminescence. Our previous studies showed that both BM and PB MNCs are not transduced by Ad.DF3-βgal.17 Moreover, γ-irradiation (2.0 Gy) of BM MNCs before incubation with Ad.CMV-βgal or Ad.DF3-βgal at MOI = 100 does not alter their tranducibility, evidenced by lack of X-Gal staining (Fig 4C). As seen in Fig 4D, 0.0001% tumor cell contamination within BM MNCs is detectable by β-gal activity.
Treatment with GCV to purge Ad.DF3-tk–transduced OCI-My5 and RPMI 8226 MM cells within BM MNCs.
Having demonstrated high transduction efficiency of adenoviral vectors in MM cells, we next examined the efficiency of purging of MM cells within BM MNCs using tk gene transduction followed by GCV treatment. Proliferation of both OCI-My5 (Fig 5A) and RPMI 8226 (Fig 5B) MM cells was correlated with cell number up to 1 × 106cells/mL. Moreover, proliferation of control (nontransduced) OCI-My5, RPMI 8226, CESS, and JY (Fig 5C through F) cells was unaffected by treatment with GCV alone. Therefore, proliferation was used as a measure of residual viable tumor cells after tk transduction and GCV treatment. Tumor cells (2 × 105) were mixed with 2 × 106 γ-irradiated normal BM MNCs and transduced with either Ad.DF3-tk (MOI = 1, 10, or 100) or with Ad.CMV-tk (MOI = 10) for 2 hours and washed out for 10 hours, followed by GCV (0 to 50 μmol/L) treatment for 36 hours. The decrease in 3H-TdR incorporation observed after GCV (50 μmol/L) treatment of Ad.DF3-tk–transduced (MOI = 100) OCI-My5 (Fig 5C) and RPMI 8226 (Fig 5D) MM cells indicates a ≥6 log depletion of these MM cell lines (Fig 5G and H, respectively). As shown in Fig 5C and D, transduction with Ad.DF3-tk at MOI = 100 (6 to 7 log depletion) was associated with more efficient purging of MM cells than at MOI = 1 (1 to 2 log depletion) at similar GCV concentrations. In addition, purging efficiency of Ad.CMV-tk at MOI = 10 was comparable to that of Ad.DF3-tk at MOI = 10. CESS and JY (Fig 5E and F) cells were similarly mixed with BM MNCs and treated with Ad.DF3-tk or Ad.CMV-tk, followed by GCV. However, neither CESS nor JY EBV-transformed B cells were depleted from BM MNCs by this treatment. These data demonstrate that Ad.DF3-tk transduction of MM cells followed by treatment with GCV is effective in selectively eradicating 6 to 7 log of contaminating tumor cells.
Treatment with GCV to purge Ad.DF3-tk–transduced OCI-My5 and RPMI 8226 MM cells within BM MNCs. To construct standard curves for measuring residual viable tumor cell contamination after purging, OCI-My5 cells (A) or RPMI 8226 MM cells (B; 0 to 1 × 106 cells) were incubated in triplicate with 3H-TdR (1 μCi) for 12 hours, harvested, and analyzed on a β-counter. OCI-My5 (C) and RPMI 8226 MM cells (D; 2 × 105 cells) were mixed with γ-irradiated (2.0 Gy) normal BM MNCs (2 × 106 cells). BM MNCs containing tumor cells were transduced with Ad.DF3-tk at MOI = 1, MOI = 10, or MOI = 100 or with Ad.CMV-tk at MOI = 10 for 2 hours, washed out for 10 hours, and treated with GCV at 0 (□), 0.5 (▨), 5 (░), or 50 (▪) μmol/L for 36 hours. 3H-TdR incorporation was measured as described above and compared with that for nontransfected tumor cell in BM MNC controls. CESS (E) and JY (F) EBV-transformed B cells, which do not express adenoviral receptors, served as negative controls. All experiments were performed in triplicate. Log depeletion of OCI-My5 (G) and RPMI 8226 (H) MM cells with Ad.DF3-tk at MOI = 100 and 50 μmol/L GCV is shown.
Treatment with GCV to purge Ad.DF3-tk–transduced OCI-My5 and RPMI 8226 MM cells within BM MNCs. To construct standard curves for measuring residual viable tumor cell contamination after purging, OCI-My5 cells (A) or RPMI 8226 MM cells (B; 0 to 1 × 106 cells) were incubated in triplicate with 3H-TdR (1 μCi) for 12 hours, harvested, and analyzed on a β-counter. OCI-My5 (C) and RPMI 8226 MM cells (D; 2 × 105 cells) were mixed with γ-irradiated (2.0 Gy) normal BM MNCs (2 × 106 cells). BM MNCs containing tumor cells were transduced with Ad.DF3-tk at MOI = 1, MOI = 10, or MOI = 100 or with Ad.CMV-tk at MOI = 10 for 2 hours, washed out for 10 hours, and treated with GCV at 0 (□), 0.5 (▨), 5 (░), or 50 (▪) μmol/L for 36 hours. 3H-TdR incorporation was measured as described above and compared with that for nontransfected tumor cell in BM MNC controls. CESS (E) and JY (F) EBV-transformed B cells, which do not express adenoviral receptors, served as negative controls. All experiments were performed in triplicate. Log depeletion of OCI-My5 (G) and RPMI 8226 (H) MM cells with Ad.DF3-tk at MOI = 100 and 50 μmol/L GCV is shown.
Effect of Ad.DF3-tk transduction and GCV treatment on the growth of normal human hematopoietic progenitor cells.
To assess the effects of Ad.DF3-tk transduction and GCV treatment on the growth of normal HPCs, BM MNCs were cultured with Ad.DF3-tk (MOI = 10) and/or GCV (50 μmol/L) and CFU-GM and BFU-E colonies were enumerated (Table 1). CFU-GM and BFU-E growth was unaffected relative to untreated control BM MNC cultures in media alone. Untreated RPMI 8226 MM cells (1%) mixed within normal BM MNCs formed a monolayer and overgrew HPC colonies. In contrast, transduction of BM MNCs containing 1% RPMI 8226 cells with Ad.DF3-tk, followed by GCV treatment, eradicated all detectable contaminating tumor cells (5 to 6 logs); importantly, this treatment does not affect growth of normal CFU-GM and BFU-E.
Detection of Ad5 E2B adenoviral DNA in Ad.DF3-tktransduced RPMI 8226 MM cells, patient MM2 cells, and normal BM MNCs before and after treatment with GCV.
To further assess the potential efficacy and selectivity of using Ad vectors for purging MM cells within BM MNCs, we transduced RPMI 8226 MM cells (Fig 6A) and patient MM2 cells (Fig6B) within normal BM MNCs (1 × 104 /sample) with Ad.DF3-tk (MOI = 100) and then treated with GCV (50 μmol/L). The presence of E2B adenoviral DNA in each sample was assessed by PCR, as in previous studies.17 28 Only RPMI 8226 MM cells (Fig 6A) and patient MM2 cells (Fig 6B) transduced with Ad.DF3-tk were positive for the E2B PCR transcript (lanes 3 and 4), whereas untransduced MM cells (lanes 1 and 2), as well as both untransduced and transduced normal BM MNCs (lanes 9 through 12) were E2B PCR-negative. Moreover, GCV treatment of Ad.DF3-tk–transduced tumor cells (lane 4) was associated with decreased PCR product, compared with Ad.DF3-tk–transduced tumor cells that were not treated with GCV (lane 3). The pattern of PCR-positivity in samples of RPMI 8226 MM cells (Fig 6A) and patient MM2 cells (Fig 6B) within normal BM MNCs (lanes 5 through 8) was similar to that observed for samples containing RPMI 8226 MM cells (Fig6A) or patient MM2 cells (Fig 6B) alone (lanes 1 through 4), consistent with the above-noted observation that tumor cells, but not normal BM MNCs, are transduced by Ad.DF3-tk (MOI = 100). Viral DNA obtained from Ad.DF3-tk particles (1 × 103 to 1 × 105 plaque-forming units [PFU]) served as a positive control forE2B PCR (lanes 13 through 15). β-actinconfirmed integrity of DNA.
Detection of Ad5 E2B adenoviral DNA in RPMI 8226 MM cells, patient MM2 cells, and normal BM MNCS transduced with Ad.DF3-tk and then treated with GCV. RPMI 8226 MM cells (A) or patient MM2 cells (B; 1 × 103/sample; lanes 1 through 4); RPMI 8226 MM cells (A) or patient MM2 cells (B; 1 × 103/sample) mixed with normal BM MNCs (1 × 104/sample; lanes 5 through 8); or normal BM MNCs (1 × 104/sample; lanes 9 through 12) were either nontransduced (lanes 1, 2, 5, 6, 9, and 10) or transduced with Ad.DF3-tk (MOI = 100; lanes 3, 4, 7, 8, 11, and 12) for 2 hours and then washed out for 10 hours. Cells were next cultured with GCV (50 μmol/L; lanes 2, 4, 6, 8, 10, and 12) or without GCV (lanes 1, 3, 5, 7, 9, and 11) for 36 hours. The E2B gene was amplified by PCR, as previously reported,17 28 from viral DNA extracted following cell lysis. Viral DNA obtained from Ad.DF3-tk particles (1 × 103 to 1 × 105 PFU) served as a positive control (lanes 13 through 15). PCR for β-actin confirmed integrity of DNA.
Detection of Ad5 E2B adenoviral DNA in RPMI 8226 MM cells, patient MM2 cells, and normal BM MNCS transduced with Ad.DF3-tk and then treated with GCV. RPMI 8226 MM cells (A) or patient MM2 cells (B; 1 × 103/sample; lanes 1 through 4); RPMI 8226 MM cells (A) or patient MM2 cells (B; 1 × 103/sample) mixed with normal BM MNCs (1 × 104/sample; lanes 5 through 8); or normal BM MNCs (1 × 104/sample; lanes 9 through 12) were either nontransduced (lanes 1, 2, 5, 6, 9, and 10) or transduced with Ad.DF3-tk (MOI = 100; lanes 3, 4, 7, 8, 11, and 12) for 2 hours and then washed out for 10 hours. Cells were next cultured with GCV (50 μmol/L; lanes 2, 4, 6, 8, 10, and 12) or without GCV (lanes 1, 3, 5, 7, 9, and 11) for 36 hours. The E2B gene was amplified by PCR, as previously reported,17 28 from viral DNA extracted following cell lysis. Viral DNA obtained from Ad.DF3-tk particles (1 × 103 to 1 × 105 PFU) served as a positive control (lanes 13 through 15). PCR for β-actin confirmed integrity of DNA.
Bystander effect after GCV treatment of tk-transduced RPMI 8226 MM cells.
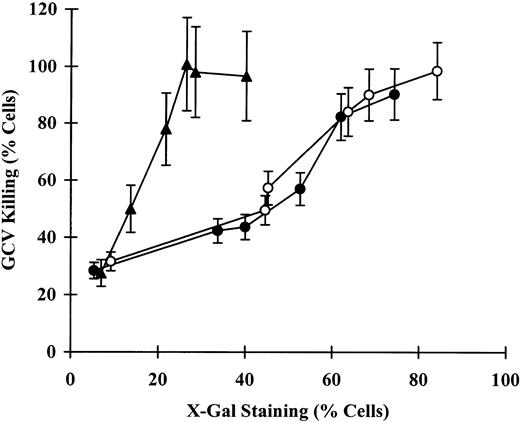
Although GCV-induced killing of tk-transduced cells may extend to proximate untransduced cells (ie, a bystander effect),33this effect has not been observed in lymphoid cells.34Nonetheless, we next determined whether GCV treatment oftk-transduced RPMI 8226 MM cells induced a bystander effect. GCV treatment of tk-transduced HeLa cells was used as a positive control for the induction of the bystander effect.34 As can be seen in Fig7, the percentage of RPMI 8226 MM cells killed by transduction with Ad.CMV-tk or Ad.DF3-tk at MOI = 1 to 100 followed by treatment with GCV cells is equivalent (P > .5) to the percentage of RPMI 8226 MM cells staining for X-Gal after transduction with Ad.CMV-βgal or Ad.DF3-βgal, suggesting the absence of a bystander effect in these tumor cells. Moreover, there was no significant difference (P > .5) in X-Gal staining or killing of RPMI 8226 MM cells transduced using CMV versus DF3 promoters. In contrast, the percentage of HeLa cells killed after transduction with Ad.CMV-tk at MOI = 1 to 100 followed by treatment with GCV was significantly greater (P < .001) than the percentage of HeLa cells transduced with Ad.CMV-βgal, confirming the presence of a bystander effect, as previously reported.34
Bystander effect after GCV treatment oftk-transduced RPMI 8226 MM cells. RPMI 8226 MM cells (3 × 104/well) were transduced with Ad.CMV-βgal or Ad.CMV-tk (•) or with Ad.DF3-βgal or Ad.DF3-tk (○) at MOI = 0, 1, 5, 10, 50, and 100 for 2 hours. Cells were washed out for 10 hours, and tk-transduced tumor cells were then treated with GCV (50 μmol/L) for 36 hours. The bystander effect was determined by comparing the percentage of transduced cells after Ad.CMV-βgal and Ad.DF3-βgaltransduction, assessed by X-Gal staining, with the percentage of cells killed after GCV treatment of Ad.CMV-tk– and Ad.DF3-tk–transduced cells, assessed by trypan blue exclusion. HeLa cervical carcinoma cells (▴), known to demonstrate the bystander effect,34 were similarly transduced with Ad.CMV-βgal or Ad.CMV-tk and served as positive controls.
Bystander effect after GCV treatment oftk-transduced RPMI 8226 MM cells. RPMI 8226 MM cells (3 × 104/well) were transduced with Ad.CMV-βgal or Ad.CMV-tk (•) or with Ad.DF3-βgal or Ad.DF3-tk (○) at MOI = 0, 1, 5, 10, 50, and 100 for 2 hours. Cells were washed out for 10 hours, and tk-transduced tumor cells were then treated with GCV (50 μmol/L) for 36 hours. The bystander effect was determined by comparing the percentage of transduced cells after Ad.CMV-βgal and Ad.DF3-βgaltransduction, assessed by X-Gal staining, with the percentage of cells killed after GCV treatment of Ad.CMV-tk– and Ad.DF3-tk–transduced cells, assessed by trypan blue exclusion. HeLa cervical carcinoma cells (▴), known to demonstrate the bystander effect,34 were similarly transduced with Ad.CMV-βgal or Ad.CMV-tk and served as positive controls.
Selectivity of the DF3 promoter in RPMI 8226 MM cells.
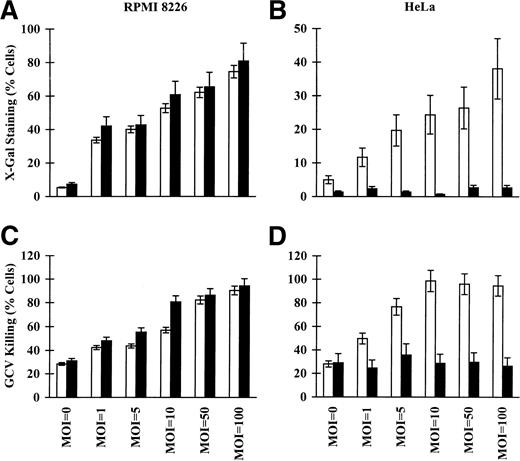
Because RPMI 8226 MM cells express DF3/MUC1 and HeLa cervical carcinoma cells lack expression of the major polymorphic MUC1/REP protein,35 we next examined the pattern of transduction of these tumor cells using the CMV and DF3 promoters. There was no significant difference (P > .5) in X-Gal staining of RPMI 8226 MM cells transduced with Ad.CMV-βgal versus Ad.DF3-βgal at MOI = 1 to 100 (Fig 8A). In contrast, a highly significant (P < .0001) difference in X-Gal staining was observed in HeLa cells transduced with CMV versus DF3 promoters at MOI = 1 to 100 (Fig8B). Importantly, no increase in X-Gal staining was observed in HeLa cells transduced with Ad.DF3-βgal at MOI = 1 to 100 (Fig 8B).
Specificity of the DF3 promoter for RPMI 8226 MM cells. DF3-positive RPMI 8226 MM and DF3-negative HeLa cervical carcinoma cells (3 × 104/well) were transduced with Ad.CMV-βgal (A and B; □) and Ad.CMV-tk (C and D, □) or with Ad.DF3-βgal (A and B, ▪) and Ad.DF3-tk(C and D, ▪) at MOI = 0, 1, 5, 10, 50, and 100 for 2 hours. Cells were washed out for 10 hours and tk-transduced tumor cells were then treated with GCV (50 μmol/L) for 36 hours. Comparison of the transduction efficiency (ie, X-Gal staining after transduction with Ad.CMV-βgal or Ad.DF3-βgal) and GCV killing oftk-transduced tumor cells (ie, viable cells by trypan blue exclusion after transduction with Ad.CMV-tk and Ad.DF3-tk followed by GCV treatment) was compared for Ad.CMV versus Ad.DF3 promoters.
Specificity of the DF3 promoter for RPMI 8226 MM cells. DF3-positive RPMI 8226 MM and DF3-negative HeLa cervical carcinoma cells (3 × 104/well) were transduced with Ad.CMV-βgal (A and B; □) and Ad.CMV-tk (C and D, □) or with Ad.DF3-βgal (A and B, ▪) and Ad.DF3-tk(C and D, ▪) at MOI = 0, 1, 5, 10, 50, and 100 for 2 hours. Cells were washed out for 10 hours and tk-transduced tumor cells were then treated with GCV (50 μmol/L) for 36 hours. Comparison of the transduction efficiency (ie, X-Gal staining after transduction with Ad.CMV-βgal or Ad.DF3-βgal) and GCV killing oftk-transduced tumor cells (ie, viable cells by trypan blue exclusion after transduction with Ad.CMV-tk and Ad.DF3-tk followed by GCV treatment) was compared for Ad.CMV versus Ad.DF3 promoters.
There was also no significant difference (P > .5) in the percentage of killing of RPMI 8226 MM cells transduced with Ad.CMV-tk and Ad.DF3-tk at MOI = 1 to 100, followed by treatment with GCV (Fig 8C). In contrast, killing after GCV treatment of Ad.CMV-tk–transduced HeLa cells was significantly greater (P < .0001) than observed after GCV treatment of Ad.DF3-tk–transduced HeLa cells (Fig 8D). Indeed, GCV treatment resulted in equivalent low-level killing of untransduced HeLa cells versus HeLa cells transduced with Ad.DF3-tk at MOI = 1 to 100 (Fig 8D), further supporting selectivity of the DF3 promoter for DF3-positive target cells.
DISCUSSION
Multiple studies have used transfection or transduction of thetk gene into target cells followed by treatment with GCV as a strategy for their selective depletion. In the context of allogeneic transplantation, for example, tk gene transduction into T cells or T lymphocyte subsets offers the possibility of abrogating GVHD in murine models as well as in humans.34,36 In MM, Dilber et al37 have used a replication deficient retroviral vector, containing the bacterial NeoR and HSV-tk fusion gene, to transduce ARH-77 and RPMI 8226 MM cells. Transgene expression after 2 weeks of G418 selection was only 13% and 9% for ARH-77 and RPMI 8226 MM cells; nonetheless, these investigators confirmed the utility of GCV treatment to eradicate tk-gene–transfected MM cells in a SCID mouse model. In the present study, we examined the feasibility of Ad vector-based strategies for delivering the tk gene, followed by treatment with GCV, for the depletion of contaminating MM cells within autologous stem cell grafts before transplantation. Although early studies suggested that transduction efficiency of Ad vectors in hematologic malignancies is low,38 more recent reports demonstrating successful Ad transduction of genes encodingβ-gal or murine CD80 into human chronic lymphocytic leukemia B cells39 suggest the potential utility of Ad gene transfer into human MM cells. In the present study, we demonstrate the presence of Ad receptors on human MM cells and that adenoviral vectors under the control of tumor selective promoters (Ad.DF3) have high transduction efficiency (80% to 100%) in human MM cells, but not in normal BM MNCs. Importantly, Ad.DF3-tk transduction followed by GCV treatment can selectively deplete ≥6 logs of MM cells, without either bystander effect or altering normal HPCs. These studies therefore suggest that tk gene transduction using Ad vectors with a tumor-selective promoter, followed by treatment with GCV, may provide a highly efficient and selective approach for the ex vivo purging of MM cells.
To test the feasibility of Ad vector-based purging of MM cells, we first needed to demonstrate the presence of functional Ad receptors on tumor cells. We showed that both MM cell lines and freshly isolated patient MM cells express the CAR adenovirus receptor, evidenced by reactivity with RmcB MoAb using indirect immunofluorescence flow cytometric analysis.18 In contrast, normal B splenocytes, CESS and JY EBV-transformed B cells, and normal BM MNCs lacked CAR expression; these observations are consistent with Ad receptor positivity being restricted to MM cells. Second, our specific radiolabeled viral binding studies confirmed this pattern of receptor expression. Third, because Ad infection is a two-step process involving attachment of virus followed by internalization mediated by αvβ3 and αvβ5integrins,29 30 we next assayed for αvβ5 expression on tumor cells and found it to be present on both MM cell lines and freshly isolated tumor cells. These observations confirmed the presence of Ad receptors on human MM cells.
To improve the selectivity of Ad vectors for human MM cells, we next used Ad vectors under the control of tumor selective promoters. In previous studies, we had shown that Ad.DF3 could be used to selectively transduce DF3-positive breast cancer cells.17 Because prior studies by others31 and by our laboratory32have demonstrated that DF3/MUC1 may also be expressed on MM cells but not normal BM plasma cells, we assayed for DF3 cell surface expression on the human MM cell lines and freshly isolated patient MM cells used in this study. Indirect flow cytometric analysis confirmed that the majority of cells expressed DF3/MUC1, suggesting the potential utility of Ad.DF3 for selectively targeting MM cells. In our study we achieved transfection using Ad.DF3-βgal equivalent to that observed with Ad vector under the control of the CMV vector (Ad.CMV-βgal), as assessed by X-Gal staining. The lack of transduction of MUC1-negative HeLa cells using Ad.DF3-βgal,even at MOI = 100, confirmed selectivity.
To directly test our purging strategy, we performed mixing experiments in which contaminating MM cells mixed with normal BM MNCs were transduced with Ad.DF3-tk and then treated ex vivo with GCV. Importantly, this strategy depleted 6 to 7 log of tumor cells, assayed first by MM cell proliferation. In both MM cell line and MM patient cells, we also used PCR to detect Ad5 E2B gene within transduced tumor cells and not normal BM MNCs and to further assess depletion of transduced cells achieved by Ad.DF3-tktransduction and GCV treatment. These data further confirm the effectiveness and specificity of this procedure for purging contaminating MM cells from normal BM MNCs. We also showed that there was no bystander effect on BM MNCs with the use of Ad.DF3-tkand GCV purging in this way. Moreover, to probe further the feasibility of using this technique for purging MM autografts, we showed that normal HPCs, assessed by BFU-E and CFU-GM, were unaffected. These characteristics suggest utility and provide the framework for testing the efficacy and safety of this method for ex vivo purging of MM cells within autografts.
Multiple other reports, as well as our prior studies in breast carcinoma, suggest that tumor cells can be effectively purged using Ad vectors without altering normal HPCs.17,40,41 However, other studies have shown that HPCs can be transduced using Ad vectors under some culture conditions.42,43 For example, entry of Ad may occur via passive mechanisms at the very high MOI (ie, 500) used in these studies, including into CD34+ HPCs that lack αv, αvβ3, or αvβ5 integrins.17 In the present study, we achieved ≥6 log depletion of MM cells under conditions that did not affect the in vitro growth of CFU-GM and BFU-E. Although our study suggests that Ad purging of MM cells is unlikely to adversely affect HPCs, this methodology must be scaled up for clinical use to evaluate not only efficacy of tumor cell purging, but also to assure that it provides for engraftment that is at least equivalent to that observed in similarly treated recipients of non–Ad-purged autografts.
What then is the role for Ad purging of tumor cells in autografting for MM? To date, a single report suggests that high-dose therapy and autografting has a superior outcome to conventional therapy3; however, all patients treated with a single transplant appear destined to relapse. Although double autografting can be safely attempted and in a retrospective analysis is superior to conventional therapy,5 its utility compared with a single autograft remains to be determined in ongoing prospective randomized trials.6 To prolong DFS, we are attempting to increase the likelihood of achieving MRD using autografting, setting the stage for the use of pharmacologic and/or immunologic approaches posttransplant to treat MRD. To address the former goal of achieving MRD posttransplant, attempts are being made to both improve ablative anti-MM therapy before transplant and to provide tumor-free autografts. Selection of CD34+ cells within autologous PBPCs can achieve a median 3.1 log reduction in tumor cell contamination, but approximately 50% CD34+ autografts still contain residual tumor cells.11,12,15,16 Depletion techniques to date using MoAbs have only achieved 2 to 3 log reduction of tumor cells in MM autografts.1,8 9 Use of Ad transduction therefore achieves levels of depletion (≥6 logs) that have not been previously attainable; it could be used alone or in combination with other purging or selection techniques in an attempt to achieve MM-free autografts for transplantation. Based on the present results, our plan is therefore to test the potential utility of Ad vector based depletion of MM cells within autografts both in terms of efficacy of ex vivo purging of tumor cells, as well as satisfactory hematologic engraftment and immunologic reconstitution in patients receiving such autografts posttransplant. Ultimately, it may be both more practical and efficient to first select CD34+ cells and then purge MM stem cell autografts using these Ad-based techniques.
Supported by National Institutes of Health Grant No. CA 78378 and the Kraft Family Reseach Fund. G.T. was supported by the Health Manpower Development Plan Fellowship, Ministry of Health, Singapore; the Medical Research Council-Shaw Medical Research Fellowship, Singapore; the Medical Research Council-Singapore Totalisator Board Medical Research Fellowship, Singapore; and the Singapore General Hospital Medical Research Fellowship, Singapore.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to Kenneth C. Anderson, MD, Department of Adult Oncology, Dana-Farber Cancer Institute, 44 Binney St, Boston, MA 02115; e-mail: kenneth_anderson@dfci.harvard.edu.