Abstract
To evaluate the role of high-dose chemotherapy (HDC) followed by autologous bone marrow transplantation (ABMT) in children with poor-prognosis Burkitt's lymphoma, the European Lymphoma BMT registry was critically reviewed. Between February 1979 and July 1991, a selected group of 89 children (78 boys and 11 girls) were considered as ABMT candidates in 12 European cancer centers for the following reasons: poor initial response (PIR) to first-line chemotherapy in 28 patients, primary refractory disease (PRD) in nine patients, sensitive relapse (SR) in 38 patients, and resistant relapse (RR) in 14 patients. The median age at ABMT was 8.2 years (range, 2.8 to 16.2 years). Thus, this report reflects data for patients surviving the salvage attempt deemed appropriate for HDC/ABMT and who then actually underwent the transplant procedure. The median follow-up period after HDC/ABMT was 4.3 years (range, 2 to 12 years). The prognosis was dismal for PRD patients and those with RR, ie, all patients died within 1 year. The 5-year event-free survival (EFS) was 56.6% (P < .0001) for patients in partial remission (PR) and 48.7% (P = .002) for patients with SR. The toxic death rate was 11.1%. Continuous complete remissions (CRs) in 39.4% of these otherwise incurable children highlight the fact that HDC/ABMT was an effective complementary procedure after conventional-dose chemotherapy protocols used during the given period. In addition, these data show that patients with PRD or RR clearly had no advantage from this aggressive and cost-intensive procedure. It has to be considered that the need for HDC/ABMT has greatly diminished in parallel with the improvement in survival using the modern intensive pulsed CCT of current protocols. To further rescue patients failing to respond to modern protocols, new approaches appear necessary, ie, combinations of HDC with antibody-targeted therapy plus allogeneic BMT for the additional benefits of the potential graft-versus-lymphoma effect.
DIFFUSE SMALL non–cleaved cell lymphoma, or lymphoblastic, Burkitt's type according to the working formulation1 or Kiel classification,2 respectively, represents the most common type of childhood non-Hodgkin's lymphoma (NHL) (almost 50%). It is characterized by the presence of B-cell markers, rapid growth, a predominantly abdominal presentation, an initial rapid response to therapy, and a tendency to early recurrence and central nervous system (CNS) involvement.3 The concept of B-cell lymphoma of childhood has developed progressively since the 1970s on the basis of both clinical and biologic criteria. It became clear that general disease control can only be achieved by early intensive multidrug pulsed chemotherapy different from those used in other NHLs.4-26 Chemotherapy is thus the cornerstone of the B-NHLs in children, and total treatment duration should not exceed 6 months. The drugs most frequently used in B-NHL treatment protocols are cyclophosphamide, vincristine, cytarabine (Ara-C), methotrexate (MTX; intravenous and intrathecal), doxorubicin, prednisone, and epidophyllotoxins. Nowadays, the prognosis of children with B-NHL is excellent, with conventional chemotherapy (CCT) reaching long-term survival rates of 95% for stage I to II, and is reported by major cooperative groups within a range of 67% to 92% for stage III to IV.6,9,10,14,16,17,19,21,23-26 The presence of CNS involvement was a major prognostic criterion, with only 30% long-term survival7,8,11 until the introduction of high-dose MTX and high-dose Ara-C along with intrathecal triple therapy, which recently improved survival probabilities up to 75% even in this former poor-risk group.10 In contrast, the role of CNS irradiation is less clear, since this modality was widely used during a period when very poor results were obtained.
Patients who fail to respond to induction therapy or who relapse after achieving a complete remission (CR) with CCT are rarely cured of their disease with CCT alone, although brief responses can be observed. With autologous bone marrow transplantation (ABMT) providing hematologic support, it has been possible to administer a high-dose chemotherapy (HDC) regimen with or without total-body irradiation (TBI) to achieve a cure in some children and adults.27 In 1978, Appelbaum et al28 first reported encouraging results using BACT (bischlorethyl-nitrosurea, cytarabine, cyclophosphamide, and 6-thioguanine) HDC followed by ABMT. However, most reports on HDC/ABMT as a potentially curative option for poor-prognosis patients focus on adult patients,27,29-45 and only some deal with the pediatric age group.46-52
Using the European Bone Marrow Lymphoma Registry, this report analyzes the largest group of children with poor-prognosis Burkitt's-type NHL (B-NHL) undergoing HDC/ABMT and tries to critically redefine the indications, values, and limitations of this procedure for the pediatric age group.
PATIENTS AND METHODS
Patients.Between February 1979 and July 1991, 89 children (78 boys and 11 girls) with poor-prognosis B-NHL underwent HDC followed by ABMT in 12 European cancer centers. The majority of patients (88%) were treated in France: 46 at the Institute Gustave Roussy/Villejuif, 29 at the Centre Léon Bérard/Lyon, and four at the Hopital Timone/Marseilles. HDC/ABMT was an accepted treatment strategy in France for high-risk cases at the given time, which was not the case in all the other European centers. Just some European transplant centers outside of France thus assumed selected patients to be eligible for HDC/ABMT. The other 12% were treated in Austria, Croatia, Italy, Israel, The Netherlands, and Spain. Thus, these patients were reported to the European Lymphoma BMT Registry on an individual basis, and reporting a case was the choice of the treating physician since this was not a prospective study but was by registration only. Patients were considered to be in the pediatric age group when the initial diagnosis was made before the age of 16 years. The median age at the time of diagnosis was 7.8 years (range, 2.3 to 15.8 years), and was 8.4 years (range, 2.8 to 16.2 years) at HDC/ABMT. The median follow-up time after ABMT is 4.3 years (range, 2 to 12 years).
Pathologic diagnosis/histology.The diagnosis in each case was based on a combination of criteria: clinical, anatomic, histologic, and cytologic, supplemented in some instances by immunologic and cytogenetic studies. Histologic features were described according to the working formulation as malignant lymphoma, diffuse, small non–cleaved cell type.
Definition of poor-risk groups.Patients with poor initial response (PIR) to first-line induction CCT either received additional surgery and/or radiotherapy to further improve the disease status or were given second- or third-line CCT before HDC/ABMT. None of these patients had reached CR by first-line chemotherapy alone, indicating a poor prognosis. Partial remission (PR) was defined as a response of at least 50%, and primary refractory disease (PRD) indicates little (<50%) or no response to induction regimens or a mixed response, ie, progression after a cycle and/or response of only short duration after a cycle.
Relapse (REL) patients presented with recurrent disease after a first CR after front-line treatments. Patients with bone marrow (BM) involvement at the time of relapse were eligible for subsequent ABMT. Seven patients were recorded with BM involvement at the time of relapse. All patients were treated according to a conventional salvage protocol, and were classified according to the response to this protocol as having either sensitive relapse (SR) with a response greater than 50% before HDC/ABMT or resistant relapse (RR) when a tumor reduction of less than 50% was achieved.
Disease status at diagnosis.All patients were staged according to Murphy's staging system.53 The disease stage at diagnosis of children in the PIR group was reported as follows: one patient had stage II, 25 had stage III, and 11 had stage IV disease (CNS and/or BM involvement). In the REL group, disease at first diagnosis was described as follows: one patient had stage I, five had stage II, 36 had stage III, and 10 had stage IV. LDH levels at diagnosis were not available in a sufficient number of patients for this report.
Prior therapy.French induction protocols were used in 77.5% of the patients. Twenty-seven patients had several courses of the COPAD regimen (cyclophosphamide, vincristine, prednisone, and doxorubicin) as induction therapy.54 The LMB 81/84 protocols were used in 33 patients.7 These protocols contain consecutive cycles of the COPAD combination plus high-dose MTX (3 g/m2) and intrathecal injections of MTX and Ara-C. Continuous intravenous Ara-C infusion (500 mg/m2) was also used in the LMB84 protocol.8 To improve the prognosis for CNS-positive and B-ALL patients, a pilot study, the LMB 86 protocol, was designed using high-dose MTX (12 g/m2), intrathecal triple therapy, consolidation with high-dose Ara-C, VP16, and cranial irradiation.9 This strategy was continued in the high-risk arm of the LMB 89 protocol.10 Ten patients were treated according to the latter two concepts. Finally, 15 patients received treatment according to BFM (Berlin-Freiburg-Münster) strategies12-15 or LSA2L2-like protocols.4,26 55 The type of first-line regimen was not reported in detail in 4 patients.
The types of treatment modalities used in the group of PIR patients and REL patients in relation to response status are given in Tables 1 and 2, respectively.
The time from first diagnosis to ABMT was less than 6 months in 27 of 37 PIR and 13 of 52 REL patients. The interval was 6 to 12 months in 10 of 37 PIR patients and 30 of 52 REL patients, whereas 9 REL patients were consolidated later than 12 months after first diagnosis.
Fifty-one patients received chemotherapy exclusively during first-line treatment. In the others, additional treatment modalities were used, including prophylactic CNS irradiation in 15, radiation to residual disease sites in 17 (7 PIR and 10 REL), and surgery on the primary tumor site in 32 (19 PIR and 13 REL). Fifty-six patients received second-line chemotherapies using either the LMB86 protocol or combinations of cisplatinum (CDDP), VP16, high-dose Ara-C, methylgag, ifosfamide, and MTX. These rescue protocols have been previously published as high-dose VP16-CDDP,56 CYVE (high-dose Ara-C and VP16),57,58 or MIME (methylgag, ifosfamide, MTX, and VP16).59 Ten patients had third-line CCT before HDC/ABMT, receiving one of the combinations outlined above but not previously used in the individual patient.
Disease status at the time of HDC/ABMT.As a result of treatment before HDC/ABMT, patients showed the following response status. Thirty-three of 89 patients were in CR as a result of various treatment modalities outlined on Tables 1 and 2, ie, 9 of 37 of the PIR group and 24 of 52 of the REL group. Fifty-six of 89 patients (28 of 37 PIR and 28 of 56 REL) still had evidence of disease at the time of HDC/ABMT. However, 13 PIR patients and 14 REL patients still responded further to additional treatments before HDC. No further response was achieved in 15 PIR patients and 14 REL patients. The size of the residual tumor mass was not consistently reported.
BM procedures.The technique of BM aspiration, cryopreservation, and reinfusion has previously been described. All marrow specimens were cytologically and histologically normal.29,34,39 All 89 patients had autologous BM reinfusions; in vitro treatment of the harvested BM was performed in 32 cases.39 60
HDC regimens.The following previously published HDC regimens were used in this patient cohort and are detailed in Table 3: BACT19,40 in 31 patients, BEAM54 61 in 23 patients, BEAC in 5 patients, BU/CY41 in 9 patients, and various others in 18 patients, including TBI in 7 patients of the latter group.
Supportive care.Patients were isolated in single rooms and received supportive care according to each institution's standards.
Statistical methods.The proportion of patients with event-free survival (EFS) until evidence of disease progression or death from toxicity related to the procedure (toxic deaths) was documented after HDC/ABMT, and was estimated by Kaplan-Meier procedures and comparison among subsets of patients determined by log-rank analysis.62
RESULTS
Response to HDC/ABMT and outcome.Nine patients of the PIR group and 24 patients with REL had reached CR with various treatment modalities before HDC. However, 56 of 89 patients still had evidence of measurable disease before HDC, ie, 19 patients were in PR, 9 had PRD, 14 had SR, and 14 had RR.
Seventeen of 28 PR-PRD patients still responded to HDC, ie, 16 with PR before HDC/ABMT achieved CR and 1 PRD patient improved to PR. The response rate was thus 61% (CR rate, 57%) in the PIR patient group. Four PRD patients showed no response. Seven early deaths occurred (2 patients with PR and 5 with PRD), and the response thus was not evaluated.
Fifteen of 28 REL patients, ie, 8 with SR and 7 with RR before HDC, achieved a second CR, whereas PR was achieved in 2 additional patients (1 with SR and 1 with RR). Thus, the response rate was also 61% with a CR rate of 54% in the REL group. Six early deaths occurred in 4 patients with SR and 2 with RR, whose response was not evaluated. No further response was observed in 1 SR and 4 RR patients.
Sixty-four patients actually were recorded as maintaining or achieving CR after HDC/ABMT. Forty-two are in continuous CR at a median of 3 years, 11 months (range, 15 months to 11 years). Twenty relapsed at a median of 11 months (range, 1 month to 3 years, 5 months), and 5 died at a median of 39 days (range, 23 to 95 days) after HDC/ABMT due to procedure-related toxicity. Only patients achieving CR before or after HDC had a chance for long-term survival.
Nineteen of 25 patients who never achieved CR died of disease progression at a median of 1 month (range, 0 to 13 months). Five of 25 died of acute transplant-related toxicity at a median of 14 days (range, 7 to 36 days), and only 1 of 25 was reported alive with stable disease 19 months after HDC/ABMT.
EFS.The actuarial EFS rates for patients with PIR after first-line treatments and REL patients was 44.9% and 35.4%, respectively, at 5 years after HDC/ABMT. The outcome after HDC/ABMT in relation to various possible prognostic factors is summarized in Table 4. Sex, age, Murphy stage at first diagnosis, type of initial CCT, number of chemotherapy courses, and type of HDC had no significant impact on prognosis in this patient cohort.
In vitro treatment of the harvested BM was performed in 32 cases. No difference in EFS was noted for both groups (P = .295). EFS was 32% and 43%, respectively, for patients with reinfusion of purged or unpurged BM.
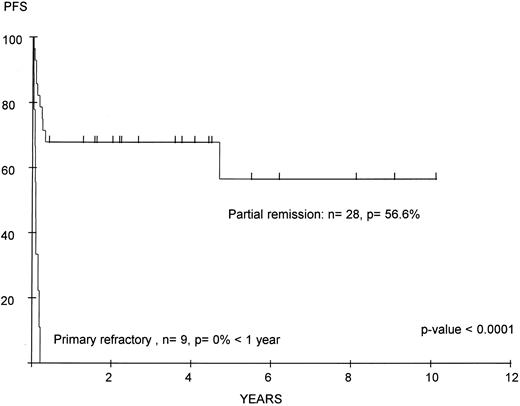
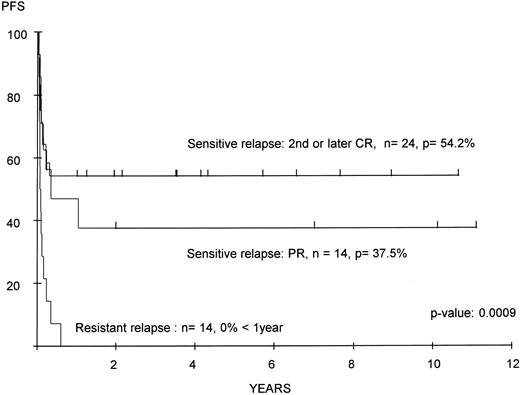
In contrast, EFS was significantly related to the response achieved by CCT before HDC/ABMT (Figs 1 and 2). None of the PRD patients were alive beyond 1 year, whereas patients with at least a PR to first-line chemotherapy still reached an actuarial EFS of 56.6% (P < .0001). Similarly, none of the patients with RR were alive beyond 1 year, but patients with recurrent disease achieving a second CR or PR (SR) achieved 5-year EFS rates of 54.2% and 37.5%, respectively (P = .0009).
EFS after ABMT of children with poor-prognosis Burkitt's lymphoma according to response to first-line conventional chemotherapy. n, number of patients; p, percentage.
EFS after ABMT of children with poor-prognosis Burkitt's lymphoma according to response to first-line conventional chemotherapy. n, number of patients; p, percentage.
EFS after ABMT of patients with recurrent Burkitt's lymphoma according to response to salvage chemotherapy for relapse. n, number of patients; p, percentage.
EFS after ABMT of patients with recurrent Burkitt's lymphoma according to response to salvage chemotherapy for relapse. n, number of patients; p, percentage.
Hematologic recovery.Hematologic recovery after HDC required a median of 17 days (range, 7 to 32 days) to reach 1,000 white blood cells, 20 days (range, 8 to 38 days), to recover 500 granulocytes, and 25 days (range, 8 to 129 days) to recover 50,000 platelets. There was no major difference in recovery times between PIR and REL groups.
Procedure-related toxicity and mortality.Sixty-four events of severe treatment-related morbidity were reported. Interstitial pneumonitis was diagnosed in 10 patients and was reported as CMV-positive in 2 patients, whereas in 8 patients no underlying cause was given. Fungal infections occurred in 5 patients (3 candida, 1 aspergillus, and 1 other). Viral infections occurred in 7 patients (herpes simplex in 2, herpes zoster in 4, hepatitis non-A/non-B in 1, and other in 1). Fever of unknown origin was reported in 37 patients. Cardiac toxicity occurred in 4 patients (2 cardiac failures, and 2 cardiac arrests), and veno-occlusive disease appeared in 1 patient. The procedure-related morbidity was thus 72% in this series.
Eight patients died of procedure-related complications: two of cardiac arrest, two of septicemia without identification of the underlying organism, one of viral infection, one of major hemorrhage, one of pulmonary complication, and one of necrotizing encephalopathy. The toxic death rate was thus 11.1% in this patient cohort.
DISCUSSION
Malignant lymphomas are among the most treatable and curable of malignant tumors, due to a unique sensitivity to chemotherapy. Unfortunately, there are still children who fail to achieve CR after front-line CCT, and about 15% are expected to relapse after having achieved CR.19 48
In this report, the results of HDC/ABMT in 89 children with poor-risk B-NHLs as reported to the European Lymphoma ABMT Registry are presented. We are aware of the potential bias adherent to any retrospective analysis. Because in this registry report information is only available for patients who survived the salvage attempt, were deemed appropriate for transplant, and then indeed underwent the transplant procedure, an estimation of the population at risk, ie, the number of initial treatment failures and relapsed patients who were started on salvage therapy with a hope for ABMT, is of interest. Apparently patients are selected since about 50% of these poor-risk B-NHL patients have been reported to escape any further dose-escalation due to rapid disease progression48 once relapse has been detected. This dropout rate was suggested by Philip et al48 when addressing the issue of salvageability in an unselected group, ie, in the French LMB84 protocol, of relapsed childhood B-NHL patients. Of 195 of 216 children achieving CR with front-line therapy, 27 had relapsed. Only 24 of 27 received rescue chemotherapy regimens, but only 15 were finally treated with HDC/CHT.
With conventional-dose cytotoxic salvage regimens, the prognosis for PIR or REL patients (children and adults) has been reported as notoriously poor with a minimal chance of cure, ie, with no more than 5% alive disease-free at 2 years.48,55,59,63 64 Therefore the potential impact of HDC/ABMT on outcome in this largest series of children with poor-prognosis B-NHL undergoing such a procedure was evaluated in aiming to critically define the future candidate within the pediatric age group.
The major determinant of survival in our study was the remission status of patients before HDC. Only children still sensitive to altered CCT had a chance to survive, ie, those showing at least a PR as a result of various primary treatments before HDC. CR after HDC/ABMT was a prerequisite for continuous remission. Forty-two of 67 children achieving CR after HDC/ABMT are in continuous CR. In contrast, patients never reaching CR did not gain any advantage from this procedure, since they all died with rapid disease progression at a median of 1 month after HDC/ABMT (range, 0 to 13 months). Thus, children with PRD or RR after the best available salvage CCT regimens prior to HDC/ABMT are not good candidates for this procedure. The results of this analysis are in line with previous reports on adult patients showing that chemoresistance is associated with a very poor outcome.27,29,33,35-38,45 48
To address the question of whether reinfusion of viable tumor cells could have influenced the outcome of these patients, the EFS of 32 patients with in vitro treatment of the harvested BM was compared with the EFS of patients receiving unpurged BM. No difference in EFS was noted for both groups (P = .295): the EFS was 32% and 43%, respectively, for patients with reinfusion of purged or unpurged BM. In this cohort, the unpurged group had a superior EFS, although statistically without any significance, suggesting that purging was preferably performed in patients with especially poor response features including minimal residual BM involvement. Thus, these registry data cannot contribute further information on the role of purging, and this question will have to be addressed prospectively. However, it should be mentioned that the first sites of relapse after BMT were the BM and CNS in two thirds of the patients.
HDC regimens were effective in this study, as demonstrated by response and CR rates in the PIR and REL groups of 61% and 54%, respectively. All HDC regimens had an equal cytoreductive potential in this patient cohort. Since the decision to use a TBI-containing regimen was not part of a prospective strategy but was the individual center's policy at the given time, 7 patients receiving TBI had shown different responses before HDC/ABMT. Since the response status was of prognostic value in this series, this would overrule any theoretic influence of TBI in this series. In addition, the number of patients was to small to demonstrate any theoretic effect. The toxic death rate of 11.1% appears acceptable in view of the intensive previous treatments and the setting of HDC/ABMT in this poor-prognosis cohort. Nowadays, some of these toxicities might be less severe since the period of BM aplasia can be shortened by the use of peripheral blood stem cell reinfusions instead of ABMT.
It appears important to focus on the various intensities of induction treatments over time. Conventional treatment with the COPAD protocol had an overall survival expectancy of only 52%.54 Relapse occurred in 25% of the patients involving the CNS, BM, and other sites not initially involved, thus demonstrating the insufficient general disease control. High-dose MTX and Ara-C were successfully used in these patients8 as salvage or second-line treatment. The major active drugs introduced in the following consecutive LMB 81/84 studies were in fact high-dose MTX (3 g/m2) and Ara-C.7,8 A major improvement was demonstrated by an EFS rate of 68% to 76% in stage IV patients without initial CNS involvement. However, the EFS for patients with CNS involvement was still only 19%. Patients on one of these protocols and/or rescue strategies, with VP16 added in some, and fitting the definition of poor-risk B-NHL still were salvaged by HDC/ABMT, as demonstrated by this study and as previously observed in a smaller subgroup of pediatric patients.47 48 In fact, this analysis showed 5-year EFS rates after HDC/ABMT for patients with initial partial response or SR of 56.6% and 35.4%, respectively. The association of a better outcome with a lower total number of treatment courses in this analysis is worth mentioning, since it reflects very well the general development in the management of this disease, namely toward fewer intensified pulsed treatment courses.
However, it is important to stress that the results were dismal for patients on the more recent LMB 86/89 protocols9 10 using high-dose MTX at 8 g/m2 and high-dose Ara-C and VP16, with no survivors after HDC/ABMT. These intensified protocols improved EFS rates in patients with CNS disease to 75%. It became clear in this cohort that patients with poor-prognosis B-NHL who failed to achieve remission with these intense induction protocols have virtually no benefit from conditioning regimens as outlined in this report. This is not too surprising, since there is no further relevant dose-escalation achieved with the HDC regimens as outlined in this report. These patients appear to need different approaches.
Thus, the reported data clearly have limitations with respect to application in the present era if highly intensive recent induction protocols are used. PRD has become numerically a more important reason for failure than relapse, and little hope is left for these types of patients. Only a completely different approach acting through a different mechanism than established multiagent chemotherapy procedures might hold hope for these types of patients. Tumor-specific targeted therapy with monoclonal antibodies has produced encouraging results in adults, with significant cytoreduction in chemoresistant patients.65-67 The Seattle group started using radiolabeled monoclonal antibodies in an ABMT setting.66 This has not yet been extensively evaluated in pediatric patients, but may well have a role in children with primary refractory B-NHL or relapse after current protocols. The source of hematopoietic stem cells might also help to improve prognosis nowadays since a significant advantage for peripheral blood stem cell support was recently reported by Voss et al,45 most likely related to the increased natural killer cell activity in the peripheral blood and the reduced risk of tumor cell contamination. Further, one could speculate as to whether such patients could benefit from the potential graft-versus-lymphoma effect associated with allogeneic BMT from related or even unrelated donors, although reports on this subject are still contradictory. Although Jones et al68 reported that relapse rates were significantly reduced, this beneficial effect was extinguished by a higher transplant-related mortality largely resulting from GVHD. However, one still has to consider that this analysis again emerges from an adult patient cohort and that GVHD risks are usually lower in the pediatric age group.69 In contrast, Chopra et al42 could not demonstrate a graft-versus-lymphoma effect in a matched-pair analysis using the adult lymphoma registry. However, the extremely poor outlook for children failing to respond to modern induction regimens appears to justify the evaluation of such an approach in a prospective manner.
Boys were much more frequently affected in this series than girls with a ratio of 8:1, which is about four times higher than observed in previous large studies.13,23 25 The median age at diagnosis was 7.8 years and thus in the expected range. However, neither sex nor age had an influence on prognosis.
Further important information emerged from the LMB84 study concerning histologic evaluation of resected residual masses at the time of assessment for CR.70 Although most often only fibrotic tissue was found, residual masses presented active disease in 25% of the patients, and survival was extremely poor in this particular group.31 Unfortunately, no histologic information was available in the 5 PIR patients undergoing surgery. Only 2 of these 5 had surgery only as a second-line procedure, whereas the other three had local irradiation in addition to surgery but no second-line chemotherapy. Since the survival estimation for these 5 CRs was 51.1%, equal to that of the PR patients without any procedure-related deaths in the CR patients, it appears unlikely that they have already been cured before HDC/ABMT. To avoid such unclear situations in the future, biopsies or resections of residual masses suspected to contain residual vital tumor cells should be performed vigorously whenever a patient appears as a candidate to be switched to second-line HDC or experimental treatment.
In summary, this study demonstrates that HDC/ABMT had high efficacy in a subset of children with poor-prognosis B-NHL who are otherwise incurable, and that toxicity was tolerable. This still may be considered if a patient with less intensive induction treatment is transferred to a cancer center with advanced disease. Otherwise, the need for HDC/ABMT has greatly diminished in parallel with the improvement in survival using the intensive pulsed CCT of current protocols. However, two indications still might be recognized nowadays: histologically proven PR after intensive induction CCT and relapse responding to salvage regimens. Because most efficient drugs are nowadays already escalated up front, the chance to add a beneficial dose-escalation with established HDC/ABMT regimens to overcome cell resistance in PR or intensively pretreated REL patients has decreased. Therefore, new myeloablative approaches appear necessary for such children, ie, combinations of HDC with antibody-targeted therapy, even in combination with allogeneic BMT for the additional benefits of the potential graft-versus-lymphoma effect. However, such questions warrant international cooperation to recruit sufficient numbers of these new poorest-risk patients.
ACKNOWLEDGMENT
The authors thank Drs Brunat, Colombat, Coze, Dini, Freycon, Huber, Laurenzi, van Leevwen, Nagler, and Nemet for entering data into the EBMT lymphoma registry.
R.L. received the Erwin Schrödinger grant when part of the work was performed.
Address reprint requests to Ruth Ladenstein, MD, St. Anna Children's Hospital, Kinderspitalgasse 6, A-1090 Vienna, Austria.