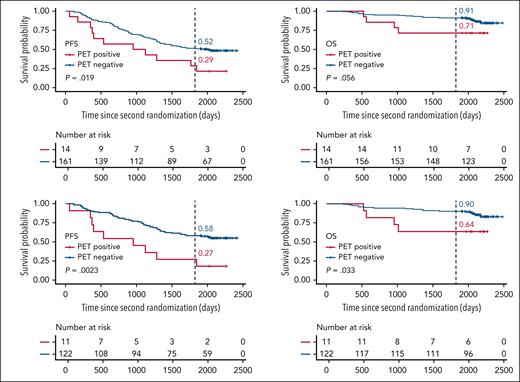
In this issue of Blood, Kraeber-Bodéré et al1 report the results of CASSIOPET, the imaging companion study of the CASSIOPEIA trial, showing that achieving negativity in positron emission tomography (PET) before initiation of maintenance therapy remains an important prognostic marker for patients with multiple myeloma (see figure).
Residual uptake in fluorodeoxyglucose-PET before initiation maintenance therapy has a negative effect on progression free and overall survival. See Figure 2 in the article by Kraeber-Bodéré et al that begins on page 3050.
Residual uptake in fluorodeoxyglucose-PET before initiation maintenance therapy has a negative effect on progression free and overall survival. See Figure 2 in the article by Kraeber-Bodéré et al that begins on page 3050.
It has been known for a long time that having multiple focal lesions of disease activity detected by advanced cross-sectional imaging like PET or magnetic resonance imaging at first diagnosis of multiple myeloma are associated with an adverse prognosis.2 Biopsies of these lesions showing differences in both the cancer cells and the microenvironment from random bone marrow samples have further emphasized that their significance goes beyond a mere reflection of a high tumor burden.3,4
Having such lesions as residuum after the most intensive part of therapy, however, might reflect not only a high initial tumor burden but to a certain degree even treatment failure.
CASSIOPEIA was a pivotal phase 3 trial which has shown the benefits of adding a CD38 antibody to induction, consolidation, and maintenance therapy in patients with multiple myeloma who are considered eligible for high-dose chemotherapy and autologous stem cell transplantation.5 Since then, further clinical trials have shown that the 2 currently available CD38 antibodies, daratumumab and isatuximab significantly improve both depth of response and survival in the up-front setting.6,7 This has led to the introduction of quadruplet therapies consisting of a monoclonal antibody, a proteasome inhibitor, an immunomodulatory drug, and a glucocorticoid into routine clinical practice in many countries even in patients, who are otherwise not considered eligible for the most aggressive treatment.
Although until a few years ago, response assessment in myeloma focused on some level of reduction of monoclonal protein in serum and urine, with these new treatments achieving anything less than minimal or measurable residual disease (MRD) negativity in the bone marrow seems unsatisfying. Recent studies have even shown that rates of MRD negativity (at levels of 10–5) >80% can be achieved.7 However, because of repeatedly confirmed higher sensitivity compared to peripheral blood, MRD still must be assessed in the bone marrow as location of the main disease burden, which has 2 major problems: (1) a bone marrow biopsy is invasive and frequent assessments are oftentimes not met with great enthusiasm by the patients; (2) sticking a needle in an easy to reach area of the bone marrow by design cannot show the whole picture of a systemic disease like myeloma and will frequently miss the aforementioned focal lesions.
In fact, although Moreau et al had shown in the IMAJEM study8 (which represented an analysis similar to CASSIOPET) that at the chosen time point after completion of the most intensive part of therapy and before initiation of maintenance treatment, 16% of patients treated with a different regimen were MRD-negative but positive in PET. In the current study, about 5% of patients still showed this constellation.
Both these studies confirm prior retrospective analyses showing that even though it becomes increasingly rare, imaging positivity after therapy remains a challenge when treating patients with myeloma.2 Residual lesions at start of maintenance in fact identify a subgroup of individuals with functional high-risk disease that might not always present as such at first diagnosis when using current risk-stratification systems. However, in the CASSIOPET study, patients with initial extra- or paramedullary disease which has always been an adverse prognostic marker, indeed showed a higher risk of being PET-positive before maintenance.
It is currently unknown if treatment of such residual lesions, for example with local radiation therapy or a different systemic therapy, would improve outcomes as it might eradicate the most treatment resistant clones. First data from the Nordic Myeloma Study Group suggest that intensifying treatment might be beneficial with 33% of patients with PET positivity before consolidation converting to PET negativity, thereafter.9 More preferably prospective trials are needed in this area.
Another open question is if standard fluorodeoxyglucose PET is the best assessment tool for myeloma. Different approaches using other tracers or functional magnetic resonance imaging have shown to be more sensitive in finding focal lesions. However, availability and financial constraints play an important role in this setting.10
In summary, CASSIOPET is confirming that even in the era of quadruplet therapy residual focal lesions in imaging before maintenance therapy are of adverse prognostic relevance for patients with multiple myeloma, even if they have achieved MRD negativity. How to respond to both MRD and PET positivity represents a medical need for future research.
Conflict-of-interest disclosure: J.H. serves on the advisory boards of Sebia, Regeneron, and Pfizer; serves on the data safety monitoring board of Janssen; gave talks for The Binding Site; and received consultancy fees from Siemens.