Key Points
Noninvasive neuromodulation of the brain's pain-processing circuits with submillimeter spatial precision can reduce pain hypersensitivity.
tFUS significantly modulates brain’s electrical rhythms of pain-related hypersensitivity in humanized sickle cell disease mice.
Visual Abstract
There is an urgent and unmet clinical need to develop nonpharmacological interventions for chronic pain management because of the critical side effects of opioids. Low-intensity transcranial focused ultrasound (tFUS) is an emerging noninvasive neuromodulation technology with high spatial specificity and deep brain penetration. Here, we developed a tightly focused 128-element ultrasound transducer to specifically target small mouse brains using dynamic focus steering. We demonstrate that tFUS stimulation at pain-processing brain circuits can significantly alter pain-associated behaviors in mouse models in vivo. Our findings indicate that a single-session focused ultrasound stimulation to the primary somatosensory cortex (S1) significantly attenuates heat pain sensitivity in wild-type mice and modulates heat and mechanical hyperalgesia in a humanized mouse model of chronic pain in sickle cell disease. Results further revealed a sustained behavioral change associated with heat hypersensitivity by targeting deeper cortical structures (eg, insula) and multisession focused ultrasound stimulation to S1 and insula. Analyses of brain electrical rhythms through electroencephalography demonstrated a significant change in noxious heat hypersensitivity-related and chronic hyperalgesia–associated neural signals after focused ultrasound treatment. Validation of efficacy was carried out through control experiments, tuning ultrasound parameters, adjusting interexperiment intervals, and investigating effects on age, sex, and genotype in a head-fixed awake model. Importantly, tFUS was found to be safe, causing no adverse effects on motor function or the brain’s neuropathology. In conclusion, the validated proof-of-principle experimental evidence demonstrates the translational potential of novel focused ultrasound neuromodulation for next-generation pain treatment without adverse effects.
Introduction
The multidimensional impact of chronic pain is closely correlated with quality of life and an increased risk of developing physical and mental health problems.1,2 Although opioids remain the mainstay for treating chronic pain, higher death rates due to drug overdoses have been recognized as a significant health crisis.3 Consequently, prioritizing nonpharmacological pain treatments becomes crucial to mitigating the risks associated with opioids, including drug abuse, overdose, and addiction,3,4 and thus neuromodulation methods have been increasingly explored.5-7 However, clinical application of these methods is constrained by invasive surgical procedures and/or challenges in stimulating specific and deeper brain structures.8,9
Low-intensity transcranial focused ultrasound (tFUS) is an emerging neuromodulation technology with unparalleled spatial specificity and penetration depth. tFUS holds promise in noninvasively modulating neuronal activities in specific brain regions10-15 and treating neurological disorders.16-18 Notably, a few approaches using tFUS have been applied to managing pain by targeting specific brain circuits: stimulating the right anterior thalamus for antinociception in healthy individuals,19 targeting the posterior frontal cortex to induce mood improvement in chronic pain patients,20 modulating thalamus and periaqueductal gray (PAG) regions to reduce heat pain response in nonhuman primates,21 and stimulating the PAG to attenuate formalin–mediated nociceptive activity in the spinal cord’s dorsal horn in rats.22 Despite these promising outcomes in pain research, several fundamental questions remain. First, it is unknown whether low-intensity tFUS stimulation applied to certain pain-processing brain circuits can effectively alter pain-related behaviors. This is crucial considering that noxious stimuli activate multiple brain areas,23,24 including the primary and secondary somatosensory cortex (S1 and S2), insula, thalamus, anterior cingulate cortex, and PAG. Second, the brain region specificity of the tFUS analgesic effect needs further investigation for quantification and validation. Third, establishing effective and safe pain management remains elusive because of the lack of translatable evidence and the limited use of pain assays in human interventional experiments.25,26 Alternatively, well-established rodent models of chronic pain in sickle cell disease (SCD), namely Berkeley (BERK) and Townes, exhibit similarity to human genetic and pathological disease, expressing over 99% human sickle hemoglobin27,28 and offering potential for translational pain research.29,30 Consequently, an urgent need arises to address the aforementioned critical aspects for an effective and safe approach to pain treatment using the humanized mouse model.
Here, we present a transformative approach using low-intensity tFUS neuromodulation for chronic pain management. We hypothesize that tFUS stimulation can modulate (ie, deteriorate or ameliorate) pain-associated behaviors triggered by noxious stimuli through modulating the activities of specific pain-processing brain circuits (Figure 1). Leveraging a custom-designed 128-element highly focused random array ultrasound transducer, we achieved high spatial specificity and focus steering capability for the small mouse brain. Then, we systematically studied the short-term and sustained effects of single and multisession tFUS stimulation on pain-associated behaviors evoked by noxious stimuli by varying parameters and targeting various brain regions. Using noninvasive ultraflexible scalp electroencephalography (EEG) recordings, we demonstrate that tFUS modulates neural oscillations in the specific pain-processing brain circuit underlying chronic pain and noxious heat stimuli. To ascertain the specificity of the tFUS modulatory effect, we conducted a comprehensive set of control experiments. Finally, behavior and histological evaluations were performed for a rigorous safety assessment.
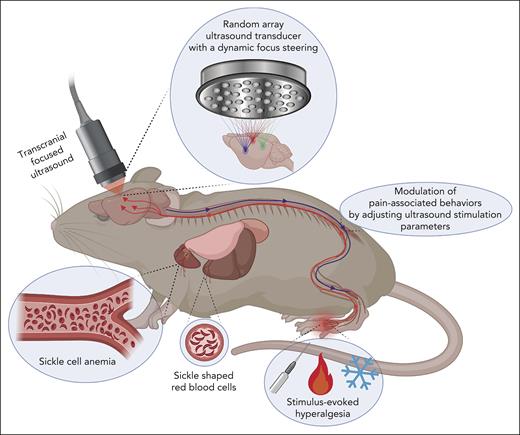
Treating chronic and stimulus-evoked hyperalgesia via tFUS stimulation to specific pain processing brain circuits. The conceptual diagram illustrates the hypothesis of treating chronic and stimulus-evoked hyperalgesia through tFUS stimulation in a humanized mouse model of chronic pain in SCD (HbSS-BERK). The modulation of pain-associated behaviors, such as amelioration or deterioration, is proposed to be achieved by selectively stimulating specific pain-processing brain circuits. This is facilitated using a 128-element highly focused random array ultrasound transducer capable of a dynamic focus steering in HbSS-BERK mice. The diagram captures the idea of targeted neuromodulation to influence pain responses in the context of SCD.
Treating chronic and stimulus-evoked hyperalgesia via tFUS stimulation to specific pain processing brain circuits. The conceptual diagram illustrates the hypothesis of treating chronic and stimulus-evoked hyperalgesia through tFUS stimulation in a humanized mouse model of chronic pain in SCD (HbSS-BERK). The modulation of pain-associated behaviors, such as amelioration or deterioration, is proposed to be achieved by selectively stimulating specific pain-processing brain circuits. This is facilitated using a 128-element highly focused random array ultrasound transducer capable of a dynamic focus steering in HbSS-BERK mice. The diagram captures the idea of targeted neuromodulation to influence pain responses in the context of SCD.
Methods
Animals
Male and female wild-type mice (C57BL/6J), male and female humanized transgenic homozygous Berkeley sickle mice (HbSS-BERK) with control homozygous normal human HbA (HbAA-BERK) mice and female HbSS-Townes mice, all bred in house, were used. HbSS-BERK mice demonstrate several features of SCD, including chronic pain, and control mice express normal human HbA (human α and β globins and no mouse globins)27,31 (supplemental Methods, available on the Blood website). All studies were approved by the institutional animal care and use committees of Carnegie Mellon University and the Long Beach VA Medical Center and complied with National Institutes of Health guidelines.
Experimental design for behavioral testing and EEG measurement
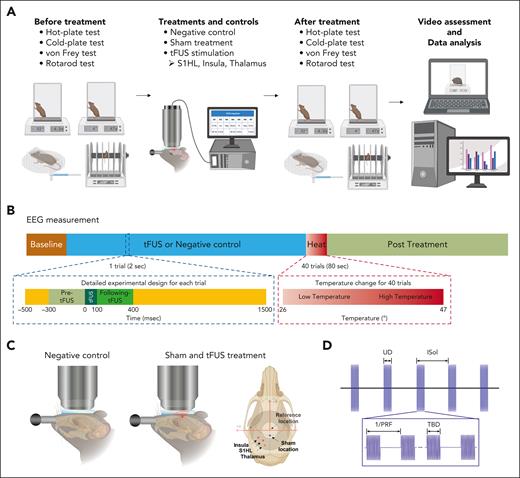
Figure 2A illustrates the behavioral experimental setup, incorporating various types of behavioral tests, tFUS stimulation using the random array transducer (H276) with multiple control groups, and video assessment with data analysis. In Figure 2B, a study paradigm for EEG measurements is presented to simultaneously investigate how tFUS stimulation influences intrinsic brain activities and heat stimulus–evoked activities where tFUS was directed onto the right hindlimb representation area of the S1 (S1HL), followed by noxious heat stimulation (≤47°C) to the plantar surface of the contralateral hind paw. Two control sets, including a negative control group (no tFUS stimulation, maintaining the same experimental procedures) and a sham-treated group (applying tFUS to a control brain structure near the bregma), were used to rule out potential confounding factors from the observed tFUS–mediated modulatory effects (Figure 2C). After characterizing the customized H276 probe (supplemental Figures 1-3), the tFUS beam was electronically steered (Table 1) and applied with controllable parameters, including a tone-burst duration (TBD) of 200 μs, pulse repetition frequency (PRF) of 40 Hz and 3 kHz, ultrasound duration of 100 milliseconds and 400 milliseconds, intersonication interval of 2 seconds and 4 seconds, and total sonication time of 10 minutes, 20 minutes, and 1 hour (Figure 2D).
Experimental design. (A) Schematic of behavioral experimental setup comprises various behavioral tests, tFUS stimulation with multiple control groups, and video assessment with subsequent data analysis. Nocifensive reactions to heat, cold, and mechanical stimuli, as well as motor performance, were recorded and evaluated to investigate the effects of tFUS stimulation at different brain locations, including S1HL, insula, and thalamus. (B) Study design for EEG measurements measurements were designed to examine both intrinsic brain activity and heat stimulus–evoked brain activity along with tFUS stimulation. (C) Control experiments were conducted to determine the specificity of the modulatory effect to tFUS stimulation at a particular brain circuit, the effects of negative control (no tFUS stimulation, maintaining experimental procedures) and sham treatment (applying tFUS to a control brain structure near the targeted brain location) were examined. (D) tFUS parameters involved customizing the 128-element random array transducer to steer ultrasound focus. Targeted brain structures were subjected to tFUS with specific parameters, including a fundamental frequency of 1.5 MHz, TBD of 200 μs, PRF of 40 Hz and 3 kHz, ultrasound duration (UD) of 100 and 400 milliseconds, intersonication interval (ISoI) of 2 and 4 second, and total sonication time of 10 minutes, 20 minutes, and 1 hour.
Experimental design. (A) Schematic of behavioral experimental setup comprises various behavioral tests, tFUS stimulation with multiple control groups, and video assessment with subsequent data analysis. Nocifensive reactions to heat, cold, and mechanical stimuli, as well as motor performance, were recorded and evaluated to investigate the effects of tFUS stimulation at different brain locations, including S1HL, insula, and thalamus. (B) Study design for EEG measurements measurements were designed to examine both intrinsic brain activity and heat stimulus–evoked brain activity along with tFUS stimulation. (C) Control experiments were conducted to determine the specificity of the modulatory effect to tFUS stimulation at a particular brain circuit, the effects of negative control (no tFUS stimulation, maintaining experimental procedures) and sham treatment (applying tFUS to a control brain structure near the targeted brain location) were examined. (D) tFUS parameters involved customizing the 128-element random array transducer to steer ultrasound focus. Targeted brain structures were subjected to tFUS with specific parameters, including a fundamental frequency of 1.5 MHz, TBD of 200 μs, PRF of 40 Hz and 3 kHz, ultrasound duration (UD) of 100 and 400 milliseconds, intersonication interval (ISoI) of 2 and 4 second, and total sonication time of 10 minutes, 20 minutes, and 1 hour.
All behavioral experiments were conducted during the light cycle of the animals and recorded on video for further validation (supplemental Methods). For heat hyperalgesia, hind paw withdrawal latency (hPWL) was determined through blind assessments. For cold hyperalgesia, hind paw withdrawal frequency (hPWF) over a 2-minute period was blindly assessed based on a prior study.31,32 For mechanical hyperalgesia, the minimum threshold of von Frey filaments was obtained using up-down method28,33 and represented as a hind paw withdrawal threshold (hPWT). Motor performance was assessed by the integral of time spent on the rod (ie, latency to fall).34 In the behavioral analysis, the unilateral effect of tFUS was assessed35 by the following metrics: Δ hPWL (seconds) = contralateral hPWL – ipsilateral hPWL, Δ hPWF = contralateral hPWF – ipsilateral hPWF, and Δ hPWT = contralateral hPWT – ipsilateral hPWT.
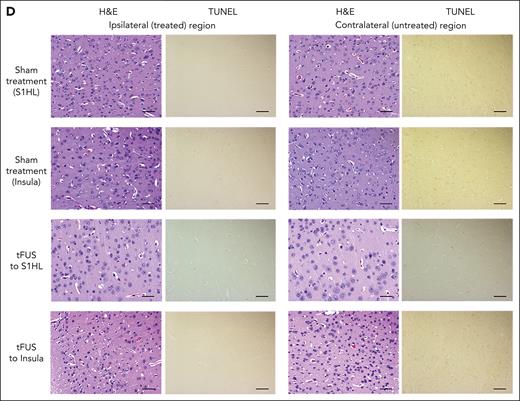
Histology
Brain sections, after a multisession treatment for 14 days with 1 hour per day, underwent staining with hematoxylin and eosin, Prussian blue, terminal deoxynucleotidyl transferase dUTP nick end labeling, platelet/endothelial cell adhesion molecule-1 (CD31), and immunoglobulin G. Blind or double-blind histological analyses were performed by a clinically qualified pathologist with expertise in sickle mice histology (supplemental Methods).
Statistics
Data are expressed as mean ± standard error of the mean unless otherwise specified, and the analyses were conducted using Prism software (GraphPad Prism, GraphPad Software, San Diego, CA) (supplemental Methods).
Results
Short-term modulation of pain-related behaviors in wild-type and SCD mice
To test the hypothesis that tFUS stimulation applied to specific pain-processing brain circuits could significantly alter thermal and mechanical sensitivity, we administered single-session tFUS stimulation with a low PRF to S1HL in wild-type mice. Previous studies demonstrated that inhibitory neuronal activities can be evoked with a low PRF condition.36 Furthermore, given the capability of the H276 device to specifically target one hemisphere of the mouse brain, we evaluated the unilateral effect of tFUS on behavioral responses to a noxious heat stimulus by comparing ipsilateral and contralateral withdrawal responses.35 The delivery of ultrasound pulses with a PRF of 40 Hz to the S1HL in the left hemisphere of the brain (Figure 3A) resulted in a significant suppression of heat pain–related behaviors in both male (Figure 3B) and female (Figure 3C) wild-type mice. This suppression is represented as a marked change in the averaged Δ hPWL for 8 minutes after tFUS compared with the baseline value, as well as sham treatment. However, Δ hPWL in the sham-treated mice did not show a significant change compared with the pretreatment baseline (Figure 3B-C).
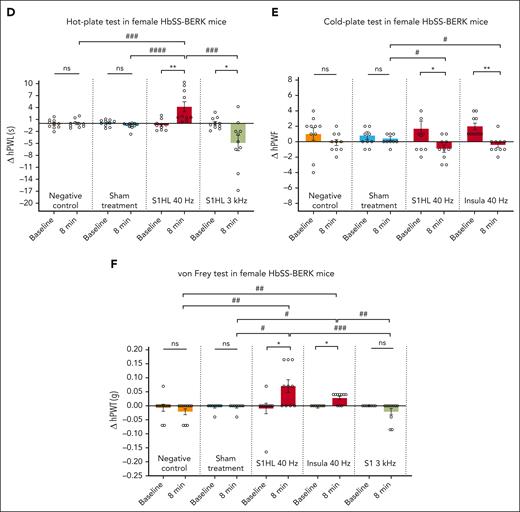
We subsequently investigated the impact of tFUS stimulation on the well-established humanized mouse model of SCD (HbSS-BERK) that constitutively displays significant thermal and mechanical hyperalgesia, which is similar to that observed in human participants with SCD.28,37 Given that higher pain intensity has been reported in females compared with males in both mice and human participants with SCD,28,32 establishing a novel pain treatment for females is of importance and priority. We evaluated responses to heat stimuli by comparing ipsilateral and contralateral hPWL values modulated by tFUS stimulation or control groups in female HbSS-BERK mice (Figure 3D; supplemental Figure 4A). Our findings indicated that a single-session tFUS with the PRF of 40 Hz applied to the left S1HL resulted in a remarkable suppression of heat hypersensitivity–related behaviors. This suppression was evident through a significant change in the averaged Δ hPWL for 8 minutes after tFUS, compared with the baseline value as well as the negative control and sham treatment. We also observed a negative value of Δ hPWL stimulated by the single-session tFUS with a PRF of 3 kHz to the left S1HL, indicating an increased contralateral hind paw hypersensitivity. Considering these distinct behavioral responses to tFUS stimulation paradigms, a bidirectional modulation of heat hypersensitivity–related behaviors was examined by adjusting PRF values to generate attenuation or exacerbation of heat hyperalgesia in female HbSS-BERK mice (supplemental Figure 8B).
Next, we investigated whether single-session tFUS stimulation could modulate cold hyperalgesia in female HbSS-BERK mice by comparing ipsilateral and contralateral hPWF values. Compared with the preapplication baseline and the sham group at 8 minutes after treatment, single-session tFUS stimulation with a PRF of 40 Hz to the left S1HL or insula led to a significant decrease in cold hyperalgesia, represented as a negative value of Δ hPWF (Figure 3E; supplemental Figure 4B).
In addition, we investigated if single-session tFUS stimulation modulates mechanical hyperalgesia in HbSS-BERK mice by comparing the withdrawal threshold between ipsilateral and contralateral hind paws (Figure 3F; supplemental Figure 4C). We found tFUS stimulation with a PRF of 40 Hz at left S1HL or insula, but not the thalamus, led to a significant reduction in mechanical hyperalgesia, indicated by a positive value of Δ hPWT, compared with the baseline as well as sham-treated or negative control mice. Similar to the exacerbation of heat hyperalgesia (Figure 3D), tFUS with a PRF of 3 kHz at the left S1HL also exacerbated mechanical hypersensitivity, represented by a negative value of Δ hPWT.
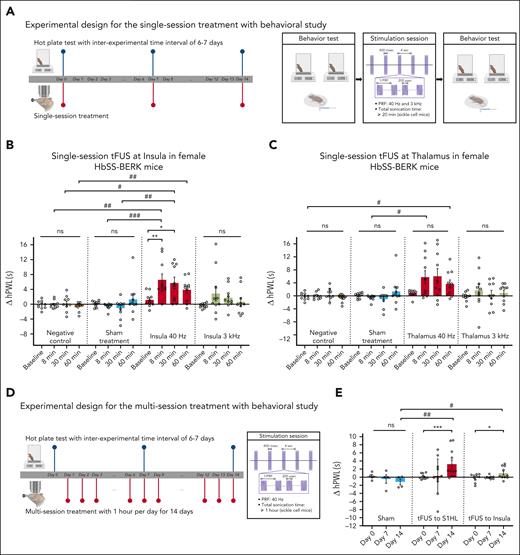
Sustained amelioration of heat hyperalgesia in sickle mice with tFUS
We investigated achieving a sustained tFUS effect on heat hyperalgesia by targeting deeper brain structures, including the insula and thalamus. The single-session tFUS with the PRF of 40 Hz at the left insula (Figure 4A) showed a much longer latency of the contralateral hind paw compared with the ipsilateral hind paw for 30 minutes, which differed from the prestimulation baseline. This effect was specific to the tFUS stimulation, as neither the control groups (negative control and sham treatment) nor tFUS with the PRF of 3 kHz significantly differed from their respective baseline values (Figure 4B). Significant differences were also observed between tFUS with the PRF of 40 Hz and controls. In contrast, delivering tFUS with the PRF of 40 Hz to the thalamus resulted in a less pronounced behavioral response with a tendency toward attenuating heat hyperalgesia (Figure 4C). Collectively, single-session tFUS stimulation with the PRF of 40 Hz to the insula, but not the thalamus, is effective for a sustained attenuation (30 minutes ≤ effect <1 hour) of hyperalgesia to heat stimuli in female HbSS-BERK mice.
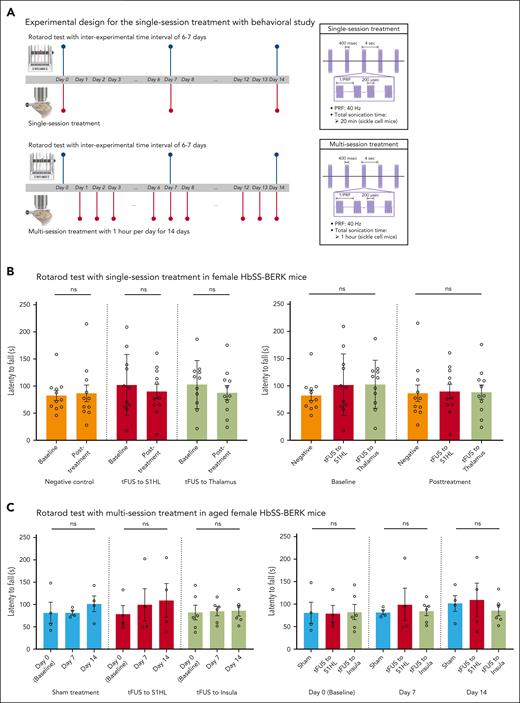
Sustained modulatory effect on heat hyperalgesia with the single- and multisession tFUS stimulation in female HbSS-BERK mice. (A) Experimental design for the single-session treatment with behavioral study. (B) The averaged Δ hPWL stimulated by single-session tFUS with a PRF of 40 Hz at left insula (n = 10) was significantly increased up to 30 minutes in HbSS-BERK mice compared with the pre-tFUS baseline, as well as values from sham (n = 10) and negative control groups (n = 10). Single-session tFUS with a PRF of 3 kHz (n = 10), sham treatment, and negative control did not result in remarkable changes in Δ hPWL compared with the baseline. ∗P < .05, ∗∗P < .01 using 1-way analysis of variance (ANOVA) with Friedman test; #P < .05, ##P < .01, ###P < .001 using 1-wayANOVA with Kruskal-Wallis test. (C) Targeting the thalamus with tFUS using a PRF of 40 Hz (n = 10) and 3 kHz (n = 10) did not result in a prominent modulatory effect compared with the prestimulation baseline, as well as sham-treated mice (n = 10) and negative control mice (n = 10), except for 2 measurements (right panel: #P = .0104, 8 minutes after tFUS with the PRF of 40 Hz and sham treatment; #P = .0277, 60 minutes after tFUS with the PRF of 40 Hz and negative control). ns, not significant, #P < .05 using 1-way ANOVA with Kruskal-Wallis test. (D) Sustained amelioration of heat hyperalgesia was examined in older female HbSS-BERK mice (10 to 15-month-old) by measuring latency to noxious heat stimuli compared with prestimulation baseline upon 14-day tFUS stimulation. (E) After multisession tFUS stimulation with a PRF of 40 Hz to S1HL (n = 11) or insula (n = 10) for 14 days, the averaged changes of Δ hPWL were significantly increased for at least 2 hours compared with the baseline values, as well as sham-treated behavioral change (n = 4). The measurement was conducted at 2 hours after tFUS or sham treatment, indicating that the effect of multisession tFUS stimulation is considered to persist for at least 2 hours. ns, not significant, ∗P < .05, ∗∗∗P < .001 using t test with Wilcoxon 1-tailed signed rank test; #P < .05, ##P < .01 using t test with 1-tailed Mann-Whitney test. ns, not significant.
Sustained modulatory effect on heat hyperalgesia with the single- and multisession tFUS stimulation in female HbSS-BERK mice. (A) Experimental design for the single-session treatment with behavioral study. (B) The averaged Δ hPWL stimulated by single-session tFUS with a PRF of 40 Hz at left insula (n = 10) was significantly increased up to 30 minutes in HbSS-BERK mice compared with the pre-tFUS baseline, as well as values from sham (n = 10) and negative control groups (n = 10). Single-session tFUS with a PRF of 3 kHz (n = 10), sham treatment, and negative control did not result in remarkable changes in Δ hPWL compared with the baseline. ∗P < .05, ∗∗P < .01 using 1-way analysis of variance (ANOVA) with Friedman test; #P < .05, ##P < .01, ###P < .001 using 1-wayANOVA with Kruskal-Wallis test. (C) Targeting the thalamus with tFUS using a PRF of 40 Hz (n = 10) and 3 kHz (n = 10) did not result in a prominent modulatory effect compared with the prestimulation baseline, as well as sham-treated mice (n = 10) and negative control mice (n = 10), except for 2 measurements (right panel: #P = .0104, 8 minutes after tFUS with the PRF of 40 Hz and sham treatment; #P = .0277, 60 minutes after tFUS with the PRF of 40 Hz and negative control). ns, not significant, #P < .05 using 1-way ANOVA with Kruskal-Wallis test. (D) Sustained amelioration of heat hyperalgesia was examined in older female HbSS-BERK mice (10 to 15-month-old) by measuring latency to noxious heat stimuli compared with prestimulation baseline upon 14-day tFUS stimulation. (E) After multisession tFUS stimulation with a PRF of 40 Hz to S1HL (n = 11) or insula (n = 10) for 14 days, the averaged changes of Δ hPWL were significantly increased for at least 2 hours compared with the baseline values, as well as sham-treated behavioral change (n = 4). The measurement was conducted at 2 hours after tFUS or sham treatment, indicating that the effect of multisession tFUS stimulation is considered to persist for at least 2 hours. ns, not significant, ∗P < .05, ∗∗∗P < .001 using t test with Wilcoxon 1-tailed signed rank test; #P < .05, ##P < .01 using t test with 1-tailed Mann-Whitney test. ns, not significant.
We further examined whether a sustained attenuation (≥1 hour) of pain behaviors could be achieved in older female sickle mice, as treatment for chronic pain in older adults is a major challenge.28,37,38 We initially observed a significant change in the behavioral response to heat stimulus, represented as the averaged hPWL, in older female HbSS-BERK mice (10 to 15-month-old) compared with those in younger female mice (5 to 9-month-old; supplemental Figure 5A). Given significantly higher heat hyperalgesia in older female HbSS-BERK mice, we administered single-session tFUS to S1HL for 20 minutes and for 1 hour, and as a result, only 1 hour of stimulation was found to produce a short-term suppression of heat hyperalgesia in older female HbSS-BERK mice (supplemental Figure 5B). Thus, to achieve a sustained effect in older female HbSS-BERK mice, we administered multisession tFUS stimulation to the selected brain regions for 14 days, with a 1-hour dose per day, on the behavioral responses to noxious heat stimuli (Figure 4D). On day 14, we observed that the effect of multisession tFUS, but not sham treatment, lasted at least 2 hours but <4 hours according to extensive behavioral assessments at 2, 4, and 6 hours after the 14-day treatment (Figure 4E; supplemental Figure 5C-D). These data suggest that 1-hour tFUS daily stimulation for 14 days with a PRF of 40 Hz at S1HL or insula can induce a sustained amelioration (2 hours ≤ effect <4 hours) of heat hyperalgesia in older female HbSS-BERK mice.
Electrophysiological evaluation and modulation of brain rhythms of pain with tFUS
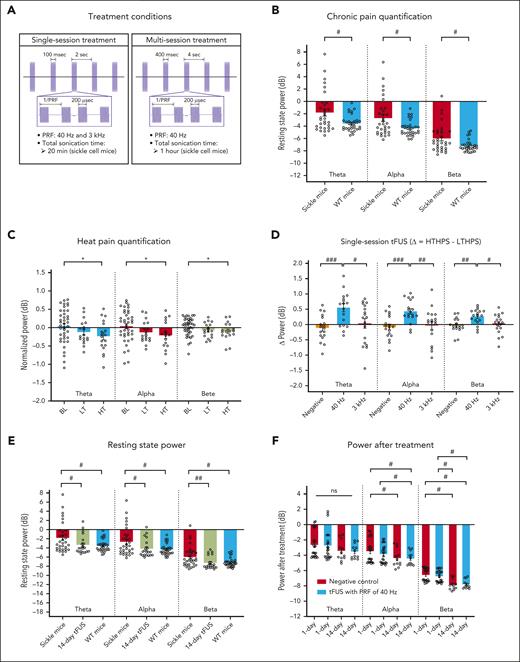
To better understand how tFUS stimulation modulates neuronal activities in the targeted brain circuits (Figure 5A), we initially quantified chronic pain based on a significant broadband increase in neuronal oscillations, spanning theta, alpha, and beta band activities in left and right S1HL (supplemental Figure 6A) of female HbSS-BERK mice compared with the power in female wild-type mice (Figure 5B). In patients with chronic pain, prior studies have demonstrated an increase in spontaneous low-frequency oscillations, particularly in theta oscillations, across various neocortical regions such as the prefrontal cortex (PFC), anterior cingulate cortex, S1, S2, and insula.39,40 Similarly, animal models of chronic pain have shown a broadband increase in oscillations spanning from theta to beta frequencies in the S1 and PFC.39-41 This increase represents a key feature of chronic pain condition, which was consistently demonstrated in the humanized HbSS-BERK mice in our EEG study. Furthermore, we found that high-temperature hind paw stimulation (HTHPS; a noxious stimulus), but not low-temperature hind paw stimulation (LTHPS; an innocuous stimulus), induced a significant decrease in theta, alpha, and beta power in the contralateral S1HL (supplemental Figure 6B) in HbSS-BERK mice compared with baseline responses (Figure 5C). This finding is consistent with previous experimental observations that noxious pain studies in human participants consistently demonstrate a suppression of low-frequency band powers, especially in the alpha and beta ranges, across cortical areas including S1, PFC, and insula.39,40,42 Leveraging the EEG pain indicators, we studied the effect of tFUS stimulation at the right S1HL on the brain rhythms underlying painful heat stimuli delivered to the plantar surface of the contralateral hind paw. After single-session tFUS stimulation with a PRF of 40 Hz, a significant increase in Δ frequency power between HTHPS and LTHPS (ie, normalized power in HTHPS – averaged normalized power in LTHPS) was observed (Figure 5D; supplemental Figure 6C-F). This distinct brain electrophysiological response to tFUS stimulation with a PRF of 40 Hz supports the observed amelioration of heat pain–related behaviors.
Modulation of heat stimulus–evoked brain activity and chronic pain resting state in female HbSS-BERK mice. (A) The single- and multisession tFUS treatment conditions used in EEG study. (B) Chronic pain quantification in brain rhythms at rest, showing a broadband increase of oscillations from theta to beta frequencies in female HbSS-BERK mice (n = 8) compared with female wild-type mice (n = 8). #P < .05 using t test with Mann-Whitney test. (C) Heat pain quantification in brain oscillations from the negative control group. HTHPS but not LTHPS resulted in a significant decrease in theta, alpha, and beta power in the contralateral brain region of S1HL in HbSS-BERK mice (n = 8). Note the temperature categories: baseline (BL), low temperature (LT; 26.2 ± 0.2°C < T ≤ 36.2 ± 0.2°C), and high temperature (HT; 38.9 ± 0.2°C < T ≤ 46.4 ± 0.1°C). ∗P < .05 using t test with Wilcoxon signed rank test. (D) Differences (Δ) of oscillatory power during normalized HTHPS and averaged normalized LTHPS. Post-tFUS with a PRF of 40 Hz, but not 3 kHz, at S1HL induced a significant increase in Δ power from theta to beta frequencies (n = 8), contrasting the heat pain–related EEG pattern. #P < .05, ##P < .01, ###P < .001 using t test with Mann-Whitney test. (E) Multisession tFUS at S1HL induced a significant decrease in power from theta to beta frequencies (n = 5), showing a remarkable difference from the power of untreated HbSS-BERK mice while being similar to the power of wild-type mice. #P < .05, ##P < .01 using t test with Mann-Whitney test. (F) At 80 seconds after heat stimulus at hind paw, power in alpha and beta frequencies was significantly suppressed by multisession tFUS with a PRF of 40 Hz but not by single-session tFUS with a PRF of 40 Hz (n = 8 for single-session tFUS and n = 4 for multisession tFUS). #P < .05 (t test with Mann-Whitney test). ns, not significant.
Modulation of heat stimulus–evoked brain activity and chronic pain resting state in female HbSS-BERK mice. (A) The single- and multisession tFUS treatment conditions used in EEG study. (B) Chronic pain quantification in brain rhythms at rest, showing a broadband increase of oscillations from theta to beta frequencies in female HbSS-BERK mice (n = 8) compared with female wild-type mice (n = 8). #P < .05 using t test with Mann-Whitney test. (C) Heat pain quantification in brain oscillations from the negative control group. HTHPS but not LTHPS resulted in a significant decrease in theta, alpha, and beta power in the contralateral brain region of S1HL in HbSS-BERK mice (n = 8). Note the temperature categories: baseline (BL), low temperature (LT; 26.2 ± 0.2°C < T ≤ 36.2 ± 0.2°C), and high temperature (HT; 38.9 ± 0.2°C < T ≤ 46.4 ± 0.1°C). ∗P < .05 using t test with Wilcoxon signed rank test. (D) Differences (Δ) of oscillatory power during normalized HTHPS and averaged normalized LTHPS. Post-tFUS with a PRF of 40 Hz, but not 3 kHz, at S1HL induced a significant increase in Δ power from theta to beta frequencies (n = 8), contrasting the heat pain–related EEG pattern. #P < .05, ##P < .01, ###P < .001 using t test with Mann-Whitney test. (E) Multisession tFUS at S1HL induced a significant decrease in power from theta to beta frequencies (n = 5), showing a remarkable difference from the power of untreated HbSS-BERK mice while being similar to the power of wild-type mice. #P < .05, ##P < .01 using t test with Mann-Whitney test. (F) At 80 seconds after heat stimulus at hind paw, power in alpha and beta frequencies was significantly suppressed by multisession tFUS with a PRF of 40 Hz but not by single-session tFUS with a PRF of 40 Hz (n = 8 for single-session tFUS and n = 4 for multisession tFUS). #P < .05 (t test with Mann-Whitney test). ns, not significant.
Furthermore, we extensively examined whether multisession tFUS demonstrating sustained suppression of pain behaviors affects the resting-state EEG power in older female HbSS-BERK mice. We measured the resting-state EEG power on the day after 14 day repeated tFUS stimulation (1-hour tFUS treatment per day) and found a significant broadband decrease in neuronal oscillatory activities ranging from theta to beta frequencies in the left and right S1HL regions compared with the power in female HbSS-BERK mice (Figure 5E). This decrease brought the oscillatory powers close to those observed in wild-type mice. In addition, we examined the impact of post-tFUS stimulation after heat stimuli and found a significant power suppression in alpha and beta frequencies compared with multi- and single-session tFUS with a PRF of 40 Hz in post-time periods of 6 minutes (Figure 5F).
tFUS safety evaluation
We assessed whether tFUS stimulation to superficial and deep brain regions would negatively affect normal motor coordination43,44 (Figure 6A). After single-session tFUS stimulation at S1HL or thalamus and multisession tFUS stimulation to S1HL or insula, we did not observe any significant difference in the averaged latency to fall on the rotarod compared with prestimulation baseline, negative control or sham treatment (Figure 6B-C). Similarly, the average time spent on the rotarod from the negative control or the multisession sham treatment was not markedly different from the baseline values, indicating that single- and multisession tFUS stimulation at cortical and deep brain structures does not induce an adverse effect on motor function in HbSS-BERK mice.
To further examine the possibility of adverse effects of tFUS stimulation, a double-blind or blind evaluation of brain histology was performed after chronic treatment (1 hour per day over 14 days) in HbSS-BERK mice and genetic control mice, HbAA-BERK (Figure 6D; supplemental Figure 7). We did not observe any significant change in the structural integrity of the tissues, iron deposits, or the number of apoptotic cells in the ipsilateral (treated) and contralateral (untreated) brains, as well as those from the sham, negative control, and multisession high-dose tFUS treatment (Figure 6D; supplemental Figure 7E-F). In addition, immunomicroscopic imaging confirmed no evidence of extraluminal immunoglobulin G extravasation or disruption of the blood vessel integrity in the studied brain sections from HbSS-BERK mice (supplemental Figure 7G).
Discussion
We have developed a novel noninvasive and nonpharmacologic tFUS neuromodulation approach as an analgesic intervention without causing adverse effects on neuropathology and brain function in preclinical mouse models of chronic hyperalgesia. We demonstrate that single- and multisession tFUS stimulation noninvasively and distinctly interacts with electrophysiological activities in pain-processing brain circuits, leading to a significant modulation of pain-associated behaviors.
Previous studies have demonstrated that optogenetic activation of parvalbumin (PV) neurons at 40 Hz or tFUS at 40 Hz in the hippocampus or S1 triggers the activation of immune cells45-47 or induces mechanical hypersensitivity,48 respectively. In contrast, vibroacoustic treatment at 40 Hz leads to a beneficial effect on chronic pain disorders, such as fibromyalgia, with widespread musculoskeletal pain.49,50 We observed that repeated ultrasound pulses at 40 Hz to multiple brain regions exhibit a distinct contrast to the brain oscillatory pattern of pain and ameliorate pain-associated behaviors. In addition to the effect of specifically repeated pulse rates, a lower duty cycle has been shown to induce inhibitory effects in cortical and thalamic neuronal activity.51,52 Thus, we further investigated whether tFUS with specific PRF values within a low-duty cycle, while maintaining the same transmitted ultrasound energy, could lead to a reduction in sensitivity to a nociceptive stimulus. Neither tFUS stimulation with additional parameter 1 (PRF, 10 Hz and TBD, 800 μs) nor additional parameter 2 (PRF, 3 kHz and TBD, 2.67 μs) resulted in a significant change in heat pain-related behaviors in HbSS-BERK mice compared with prestimulation (supplemental Figure 8A). In addition, we adjusted PRF values from 40 Hz to 3 kHz, which results in changes to spatial peak temporal average (SPTA) intensity (ISPTA) values from 2.02 to 208.46 mW/cm2, and found that tFUS with a PRF of 1 kHz, corresponding to ISPTA of 50.53 mW/cm2, can be considered as a turning point from generating neural inhibition (suppressing pain-related signals) to inducing neural excitation (intensifying pain-related signals) when tFUS is applied to S1HL (supplemental Figure 8B). Thus, the ultrasound PRF value plays a key role in modulating behavioral responses to noxious stimuli in HbSS-BERK mice. We also found a remarkable change in brain oscillations stimulated by the single-session tFUS with PRF of 3 kHz to the S1HL from the innocuous LTHPS period (supplemental Figure 6C-F), which is a completely different response to the tFUS with PRF of 40 Hz showing a significant increase in frequency power from HTHPS period (Figure 5D). This distinct pattern may be induced by facilitated cortical excitability53 built up during the excitatory tFUS neuromodulation with PRF of 3 kHz (supplemental Figure 6G-I). This finding is consistent with prior studies demonstrating the critical contribution of CaMKIIα on chronic pain exaggeration in HbSS-BERK mice,30,54 increased power in low-frequency bands by optogenetically suppressing, for example, cortical PV inhibitory neurons,53 and tFUS–mediated distinct action potential waveforms and significant spike rates of S1 in transgenic CaMKIIα mice and PV mice.36 Hence, further studies to investigate the effects of tFUS stimulation at both low and high PRF levels are necessary to delineate the neuromodulation impact on specific neuronal activities in the presence of the innocuous and noxious stimuli.
We conducted a comprehensive set of control experiments to evaluate whether the achieved analgesic effect is specific to tFUS stimulation. First, to prevent the potential analgesic effect of anesthesia, we used an awake experimental setup (ie, a head-restrained awake naturally walking mouse in the air-lifted platform) to directly measure the tFUS modulatory effect (supplemental Figure 9A-B). As we also observed a consistent and significant tFUS modulatory effect in head-fixed awake mice, the light anesthesia used in this study does not confound the conclusion that tFUS can modulate pain-associated behavioral responses. Second, considering the possibility of altered nocifensive behaviors in the repeated hot-plate test due to nonnociceptive factors such as learning or habituation,55,56 we examined the effect of interexperimental day intervals to rule out the potential contribution of nonnociceptive factors to the observed tFUS–mediated analgesic effect (supplemental Figure 9C). After measuring latency from noxious heat stimuli every 3 to 4 days (but not 6-7 days), we observed a significant decrease in the hPWL from the measurement on days 10 to 11 compared with the hPWL on day 1 in HbSS-BERK mice. This suggests that an interexperimental time interval of 6 to 7 days can minimize the impact of nonnociceptive factors on the pain-related behaviors modulated by tFUS.
For clinical translation, low-intensity ultrasound (ISPTA: 208.46 mW/cm2 at the highest PRF of 3 kHz and 0.35 W/cm2 at the TBD of 200 μs measured behind a freshly excised female mouse skull sample) was used to adhere to the regulatory standards for diagnostic ultrasound safety (ISPTA ≤ 720 mW/cm2; ISPPA ≤ 190 W/cm2) set by the US Food and Drug Administration.57,58 We further investigated the impact of tFUS on heat pain-associated behaviors in female HbAA-BERK control and HbSS-Townes mice. Notably, single-session tFUS with a PRF of 40 Hz significantly suppressed heat pain-related behaviors in female HbAA-BERK control mice (supplemental Figure 10A) and female HbSS-Townes mice (supplemental Figure 10B). In particular, with different globin chains32 and fetal hemoglobin levels closely related to patterns of pronociceptive and antinociceptive brain connectivity in Townes sickle mice,59 this may contribute to more gradual tFUS effects on pain behaviors compared with the more spontaneous tFUS effects observed in BERK mice. In addition, the efficacy of single-session tFUS with a PRF of 40 Hz to S1HL or insula was remarkably diminished in older female and male HbSS-BERK mice (supplemental Figure 11A-D), as well as older female wild-type mice treated by tFUS to S1HL given their remarkably increased heat pain sensitivity (supplemental Figure 11E-F). Notably, this dosage window appears to be less dependent on sex differences (supplemental Figure 11A-D) compared with the sex-dependent variations observed in response to N-methyl-D-aspartate receptor antagonist60 and ketamine administration.61 Pain and cognitive impairment often coexist in conditions like SCD, and older individuals with SCD experience an increase in pain28,29; and older sickle cell mice display cognitive and neurobehavioral deficits not observed in their younger counterparts.62 Indeed, our observations support this notion, as we found that increasing the dosage of ultrasound stimulation led to a significant (Figure 5B) and sustained (Figure 4E and 5C-D) reduction in pain-related behaviors in aged sickle mice that showed significantly higher heat hyperalgesia (Figure 5A). Hence, these observations highlight the need to establish a patient-specific dosage window for tFUS stimulation, considering age and/or interindividual variability. Based on the histological investigations, we established an extended safety window for tFUS stimulation using high-dose tFUS stimulation (transcranial peak-peak pressure, 2059.75 kPa; ISPTA, 262.30 mW/cm2 at the PRF of 40 Hz and 32.79 W/cm2 at the TBD of 200 μs measured behind a freshly excised female mouse skull sample) to prevent short- and long-term adverse effects.
From a neuromodulation perspective, further studies are necessary to clarify the mechanisms behind the potential implications of chronic pain, specifically focusing on the observed results of the significantly modulated resting-state brain rhythms induced by 14-day stimulation in HbSS-BERK mice. Central sensitization, defined by the amplification of neural signaling within the spinal cord30,63 and greater activation in the brain regions,63 including the brain stem, thalamus, and cortex, is recognized as 1 of the key mechanisms in perpetuating persistent pain hypersensitivity in SCD.59,64 We provide proof for the first time that directly targeting specific pain-processing circuits in the brain leads to a significant change in pain-related behaviors in the humanized HbSS-BERK mice. Furthermore, the promising evidence of suppression of heat pain–associated behaviors, along with a significant change in the brain rhythms after single- and multisession tFUS stimulation (Figure 5D-F), not only warrants further investigation into the efficacy of single- and multisession tFUS beyond the 14-day period but also necessitates neurobiological assessments of the induced long-lasting analgesic effects. This novel tFUS neuromodulation technology in the context of SCD may be acting on or via one or multiple neurochemical pathways, such as the top-down inhibitory pain pathway along with the serotonergic or dopaminergic system, for targeting complex central nervous system–based nociceptive mechanisms induced by the noxious SCD microenvironment replete with inflammation, oxidative stress, and neural injury. Due to the complexity of the neurobiology of pain in SCD and the preliminary nature of our preclinical findings in a humanized mouse model of chronic pain in SCD in vivo, our results do not indicate that human patients will readily benefit from this technology, but rather justify the necessity of undertaking large-scale clinical studies. In addition, exploring the impact of simultaneously targeting multiple pain-processing brain circuits, for example, costimulations at S1 and insula, may reveal the potential for generating more amplified inhibitory effects on pain-associated behaviors than respective S1 or insula stimulation alone.
The preclinical results presented here showcase a unique bidirectional modulation of pain-associated behaviors through tailored tFUS stimulation, using both effective and ineffective PRF. To successfully conduct clinical translation, further studies are necessary to clarify the mechanisms behind the potential implications of modulated pain-related behaviors in sickle cell mice. Previous studies have underscored the antinociceptive properties of pharmacological interventions such as duloxetine,65 dexmedetomidine,66 ceftriaxone,67 and antiepileptics with selective serotonin reuptake inhibitors68 for reducing pain-related behaviors and pain in sickle cell mice and individuals with SCD, respectively. In particular, the prior research65 using duloxetine suggests that targeting the descending serotonergic pathway in sickle mice could be a potential treatment for individuals experiencing pain associated with SCD. Similarly, low-intensity tFUS stimulation may trigger the descending pain modulatory system in sickle cell mice. To be specific in our study, we postulate that the inhibitory effects of tFUS using a PRF of 40 Hz at the S1HL may affect the descending pain inhibitory projections to the spinal cord. Therefore, leveraging this previous pharmacological research as a benchmarking reference could aid in the development of effective pain treatment strategies. In addition, applying the ultrasound PRF of 40 Hz for inhibitory effects would be recommended, and the effective and safe tFUS stimulation parameters, including ISPTA (2.02 mW/cm2 at the PRF of 40 Hz and 0.35 W/cm2 at the TBD of 200 μs), can be properly scaled up from small animal brains to human brains. In addition, it is essential to consider that modifying the ultrasound’s fundamental frequency from 1.5 MHz to hundreds of kHz and increasing ultrasound intensity may be necessary to effectively modulate larger human brain targets when accounting for thick human skulls. Additional details for discussions are available in the supplemental Information. Additional data can be found in the public repositories listed in the Footnotes.
In summary, our study marks the first demonstration of the significant impact of noninvasive low-intensity tFUS stimulation on brain oscillations and thermal and mechanical pain-associated behaviors in in vivo mouse models by targeting cortical and deep brain structures associated with pain processing. The experimental evidence presented, coupled with the significant advancements in the efficacy and safety of tFUS neuromodulation using a state-of-the-art multielement highly focused random array transducer, underscores the translational potential as an effective, nonpharmacological, and noninvasive device–based neuromodulation for managing pain.
Acknowledgments
The authors thank Natalie Garcia and Reina Lomelli, University of California, Irvine, for their effort for breeding transgenic mice. The authors also thank Kyle Morrison from Sonic Concepts, Inc for providing consultation in customizing the H276 probe.
This work was supported in part by National Institutes of Health (NIH) grants EB029354 (National Institute of Biomedical Imaging and Bioengineering), NS124564 (National Institute of Neurological Disorders and Stroke), NS131069 (National Institute of Neurological Disorders and Stroke), HL147562 (National Heart, Lung and Blood Institute), and CA263806 (National Cancer Institute). S.K. was supported by Diversity Supplement grant 3R01HL147562-03S; and D.A. has been supported by a University of California President's Fellowship, Giannini Foundation Fellowship, and NIH grant K99 AT012494-01A1 (National Center for Complementary and Integrative Health).
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Some illustrations in figures and supplemental figures were created with BioRender.com.
Authorship
Contribution: B.H. and K.Y. initiated the concept; B.H., K.Y., M.G.K., and K.G. designed the studies; M.G.K. conducted behavior experiments with neuromodulation and analyzed behavior data; M.G.K. and C.-Y.Y. performed electroencephalography experiments with neuromodulation and analyzed electrophysiological data; K.Y., Y.N., C.-Y.Y., and D.A. conducted behavior data assessments; K.G., D.A., and S.K. produced sickle cell mice; K.Y., K.K., and Q.C. designed the multi-element array transducer; K.Y. simulated the design of random array ultrasound transducer in experimental setup; K.Y., M.G.K., and X.N. characterized the transducer array and validated the ultrasound targeting; R.F. and D.A. performed histology assessments; M.G.K. and K.Y. wrote the original draft; B.H., K.G., R.F., D.A., C.-Y.Y., K.K., Q.C. and Y.N. contributed to reviewing and editing of the manuscript; and B.H. and K.G. supervised the work.
Conflict-of-interest disclosure: B.H., K.Y., and X.N. are coinventors of pending patent applications on transcranial focused ultrasound technique. K.G. received honoraria from Novartis and CSL Behring; and research grants from Cyclerion, 1910 Genetics, Novartis, Grifols, Zilker, and University of California, Irvine Foundation. The remaining authors declare no competing financial interests.
Correspondence: Bin He, Department of Biomedical Engineering, Carnegie Mellon University, 5000 Forbes Ave, Pittsburgh, PA 15213; email: bhe1@andrew.cmu.edu.
References
Author notes
M.G.K. and K.Y. contributed equally to this study.
Data supporting the conclusions are presented in the article and supplemental Information. Additional data can be found in Figshare repository at: Computer simulations of the 128-element random array ultrasound transducer (ie, H276): https://doi.org/10.6084/m9.figshare.25036364.v1; Ex-vivo characterization of the H276: https://doi.org/10.6084/m9.figshare.25036925.v1; Behavioral assessment with analysis: https://doi.org/10.6084/m9.figshare.24867198.v1; EEG data: https://doi.org/10.6084/m9.figshare.24867261.v1; Intracranial recording data: https://doi.org/10.6084/m9.figshare.25006955.v1; Histology images: https://doi.org/10.6084/m9.figshare.25006901.v1.
The online version of this article contains a data supplement
There is a Blood Commentary on this article in this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.