Plasma cells are specialized immune cells that can survive in the bone marrow for decades and continually secrete large amounts of antibodies, thus providing long-term, often lifelong protection from repeated exposures to a pathogen. The long-term survival and the capability to secrete high amounts of protein make plasma cells a potential candidate for stable delivery of therapeutic proteins and antibodies. However, engineering plasma cells or B cells has been challenging due to low lentiviral transduction efficiency, incompatibility with plasmid transfection and loss of episomal DNA expression over time. We have previously shown that human plasma cells can be engineered to secrete antibodies and proteins in in vitro culture systems via gene editing. In the current study, we have generated engineered murine plasma cells that can secrete the clotting factor IX (FIX). We hypothesize that the FIX-secreting plasma cells will engraft long-term in FIX-deficient immunocompetent mice and secrete therapeutic levels of FIX leading to protection from Hemophilia B.
The standard of care for Hemophilia B is repeated intravenous infusion of recombinant FIX or AAV-based gene therapy. However, 30-60% humans have pre-existing immunity to AAV-based gene therapy and gene therapy can induce an immune response in people lacking pre-existing antibodies. Moreover, gene therapy is unsuitable for pediatric patients due to their rapid growth and proportional loss of AAV. Plasma cell-based therapy is lowly immunogenic and can be used for redosing in pediatric patients that require more product with age. Here, we will describe proof-of-concept studies showing that engineered murine plasma cells can engraft into immunocompetent mice without the need for conditioning and produce stable levels of protein for >10 weeks.
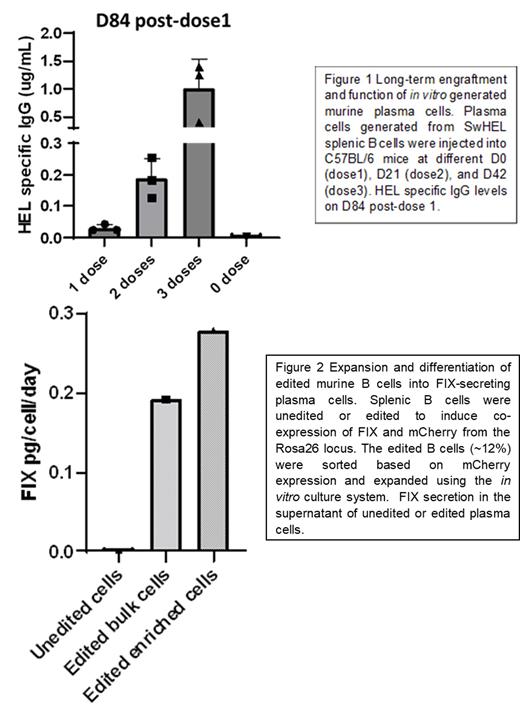
We developed a three-step in vitro co-culture system that can be used to engineer and differentiate naïve B cells into plasma cells. These in vitro generated murine plasma cells had a comparable gene expression profile and phenotype to natural plasma cells and can engraft stably, in the absence of conditioning, into immunocompetent mice whereupon they secreted antibodies (Figure 1). Moreover, we show that plasma cells can be re-dosed to increase antibody levels without triggering a secondary immune response (Figure 1).
For delivery of therapeutic proteins, we have developed adeno-associated virus-based homology directed repair reagents to edit murine B cells at several loci, including beta-2 microglobulin, Rosa-26, and the antibody heavy chain. By co-delivery of cis-linked fluorescent markers, we were able to sort and expand only edited cells, enabling enrichment of cells expressing a therapeutic protein. In proof-of-concept studies, we have used this approach to generate a human FIX-secreting plasma cell product with close to 90% edited cells at the end of the B cell culture. The enriched plasma cells generated 0.28 pg FIX/cell/day compared to 0.19 pg FIX/cell/day generated by the bulk edited cells (figure 2). We estimate that engraftment of 1 million edited plasma cells is sufficient to generate therapeutic levels of FIX upon (figure 2).
We have developed reagents for a novel cell-based therapeutic tool with protein secretion capabilities and far-reaching applications. Out studies will provide insights into the feasibility and efficacy of a B cell based therapeutic product.
Disclosures
Rawlings:Be Biopharma: Consultancy, Current holder of stock options in a privately-held company, Research Funding. James:Be Biopharma: Consultancy, Current holder of stock options in a privately-held company, Research Funding.