Background: Polycythemia vera (PV) is characterized by dysregulated Janus kinase (JAK) activation, leading to excessive production of blood cells, increased risk of thrombotic and hemorrhagic events, and an impairment on the quality of life of patients. Ruxolitinib, a JAK1/JAK2 inhibitor, has shown promising results in recent trials, but its comparative efficacy to best available therapy (BAT) remains unclear. We aimed to perform a systematic review and meta-analysis comparing the efficacy and safety of Ruxolitinib versus BAT for patients with PV.
Methods: We systematically searched PubMed, Embase, and Cochrane Central for clinical studies published up to July 1st comparing Ruxolitinib to BAT. BAT was defined as hydroxyurea, interferon or pegylated interferon, pipobroman and anagrelide. Efficacy outcomes assessed were complete response to therapy and reduction in the Myeloproliferative Neoplasm Symptom Assessment Form (MPN-SAF) score; safety outcomes were thromboembolism, anemia, and herpes. We pooled outcomes as risk ratios (RR) with 95% confidence intervals (CI). Statistical analysis was performed with Review Manager version 5.4.1. Heterogeneity was assessed with I² statistics. The protocol was registered in PROSPERO (ID: CRD42023427977).
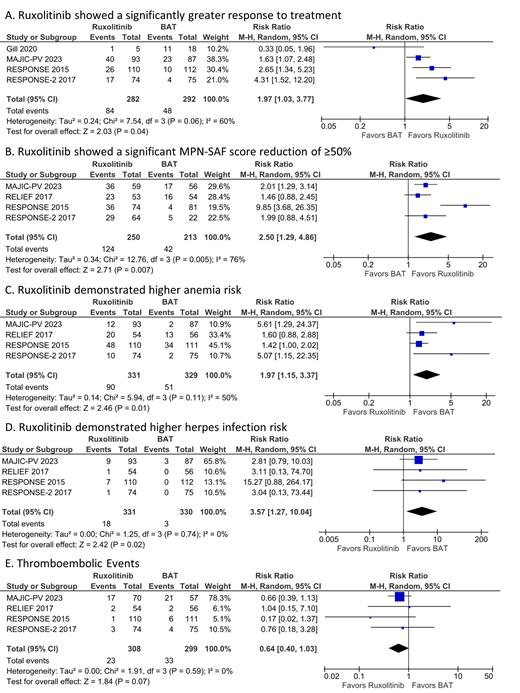
Results: A total of five studies met our inclusion criteria, of which four were randomized trials. Our analysis encompassed a population of 684 patients, including 336(49%) allocated to the Ruxolitinib group, and 348(51%) allocated to the BAT group. Ruxolitinib had a significantly greater response to treatment compared to BAT (RR 1.97; 95% CI 1.03 -3.77; p=0.04; I²=60%; Fig 1A) and significantly reduced MPN-SAF score by at least 50% (RR 2.50; 95% CI 1.29-4.86; p=0.007; I²=76%; Fig 1B). Additionally, use of Ruxolitinib showed a significantly higher incidence of herpes infection (RR 3.57; 95% CI 1.27 -10.04; p=0.02; I²=0%; Fig 1C) and anemia (RR 1.97; 95% CI 1.15-3.37; p=0.01; I²=50%; Fig 1D). There were no significant differences between the two treatment groups regarding thromboembolic events (p=0.07; Fig 1E).
Conclusion: Our meta-analysis reveals that Ruxolitinib exhibits superior efficacy in achieving a complete response for PV patients compared to BAT and in reducing MPN-SAF score by ≥50%. While no significant difference was observed in thromboembolic events, Ruxolitinib demonstrated significant risk of anemia and herpes infection.
Disclosures
No relevant conflicts of interest to declare.