Purpose/Objective:
The implications of COVID-19 induced hypercoagulability in patients with sickle cell disease (SCD) remain largely unknown. Both COVID-19 and SCD have independent pathophysiological mechanisms which impact each aspect of Virchow's triad to induce a hypercoagulable state (Saxena and Muthu., 2023), however the joint impact of COVID-19-SCD on venous thromboembolism (VTE) remains understudied. As such, our primary objective involved investigating the incidence of VTE events in SCD patients with COVID-19. Our secondary objective involved assessing parameters of COVID-19 infection severity in SCD patients.
Methods:
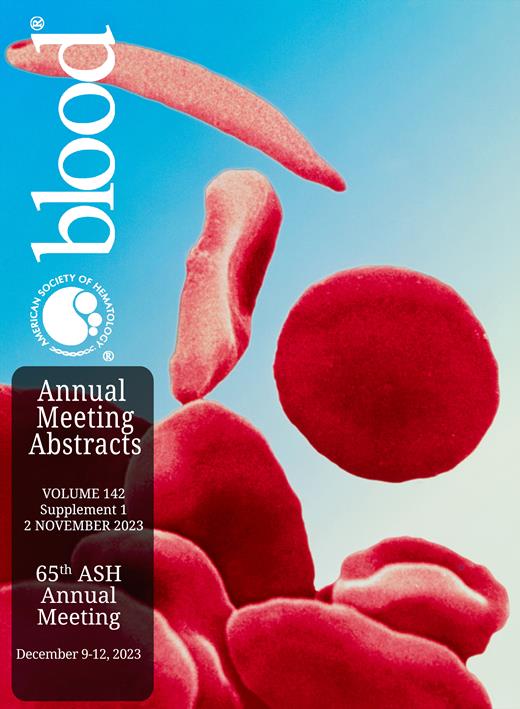
We conducted a retrospective cross-sectional study at New York City Health and Hospitals, Kings County involving SCD, sickle cell trait (SCT) and the general population of COVID-19 patients (non-sickle). Data was collected from the onset of the pandemic on March 1, 2020 to December 31, 2021 for hospitalized and intensive care patients. We collected information on incidence of VTE, type of VTE (deep vein thrombosis or pulmonary embolism), age, sex, comorbidities, VTE prophylaxis, D-dimer, ferritin, LDH, BMI, sickle cell phenotype, transfusion requirements, COVID-19 management, SCD management, and outcomes. Data was analyzed on GraphPad PRISM, using one-way ANOVA and odds ratios. A p-value of <0.05 was considered statistically significant.
Results:
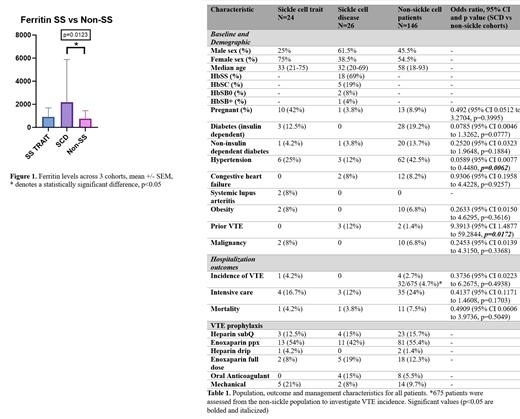
The study included three patient cohorts, consisting of 24 SCT, 26 SCD and 675 non-sickle patients (non-SS) to study incidence of VTE. Additional information regarding infection parameters was obtained on 146 non-sickle patients, and all SCT and SCD patients. We found that there was no significant difference between VTE risk in the SCD and non-sickle patients (OR=0.3736, 95% CI 0.0223 to 6.2675) or SCT and SCD patients (OR=0.2956, 95% CI 0.0115 to 7.6121). There was no significant difference in mortality (OR=0.4909, 95% CI 0.0606 to 3.9736) or intensive care requirements (OR=0.4137, 95% CI 0.1171 to 1.4608) between SCD and non-SS patients (Table 1). We also investigated markers of infection and hypercoagulability and found that there was no significant difference between D-dimer or LDH levels between the three cohorts, however ferritin was significantly increased in the SCD group compared to the non-sickle cohort (Figure 1, p=0.0123).
Conclusions/Implications:
Current ASH guidelines recommend use of prophylactic dose anticoagulation for critically ill COVID-19 patients and therapeutic dose anticoagulation for acute, but not critically ill patients (Cuker et. al., 2022). There are currently no formal recommendations regarding VTE prevention for hospitalized SCD patients with COVID-19. Our data supports prior reports on VTE in SCD (Singh et. al., 2022) which note that SCD patients with COVID-19 do not have an increased risk of VTE compared with uninfected SCD patients. Similarly, our data suggests that there is no statistical difference in VTE incidence in SCD-COVID-19 patients compared to the general population affected by COVID-19. Given no differences in VTE incidence, we recommend that anticoagulation parameters for the general population of hospitalized and intensive care patients be applied to SCD patients.
Disclosures
No relevant conflicts of interest to declare.