Abstract
Introduction
Racial and ethnic disparities are well documented in cancer patients (pts) in the United States (US). Though outcomes in relapsed or refractory acute lymphoblastic leukemia (RR ALL) have improved in recent years with the approval of novel immunotherapies including bispecific T cell engagers, antibody-drug conjugates, and chimeric antigen receptor T cells, identifying disparities in access to innovative therapies is critical. We aimed to identify novel therapy utilization, health resource utilization (HRU), and cost variations by race/ethnicity in adult RR ALL pts.
Methods
We identified two cohorts of adult RR ALL pts who received first salvage therapy (S1) since January 1, 2014 from the CMS 100% Medicare fee-for-service (FFS) beneficiaries with hematologic cancer (2007-2019) and the Optum Clinformatics Data Mart (2007-2021) databases. Pts were required to have continuous coverage with Medicare FFS or commercial insurance from 6 months before ALL diagnosis through S1 initiation. Follow-up started at S1 initiation and ended at the earliest of death, disenrollment, or 12/31/2019 (Medicare) or 3/31/2021 (Optum). Race/ethnicity was categorized as Non-Hispanic White (NHW) vs. Non-White (NW) (Black, Asian, North American Native, Hispanic). Novel therapies included blinatumomab or inotuzumab ozogamicin (no tisagenlecleucel captured in either cohort). Treatment regimens at S1 were categorized as novel therapies (with/without chemotherapy/TKIs), chemotherapy (with/without TKIs, but no novel therapies), and TKIs alone. All-cause and ALL-related HRU and costs were tallied during the follow-up period. Healthcare allowable amount was reported as total costs per patient per year (PPPY) and were standardized to 2019 US dollars.
Results
We analyzed 682 Medicare and 222 Optum RR ALL pts initiating S1 with 80% and 63% being NHW, respectively (Table 1). Pts identified in Medicare were older (median age, 71 vs. 57 years) and had more baseline comorbidities (Quan-CCI, 37.4% vs. 9.5%) than pts identified in Optum. Median follow-up time was shorter for Medicare NW pts compared with NHW pts (346 vs. 370 days), but longer for Optum NW pts (509 vs. 353 days). In the Medicare cohort, NW pts were younger (median age, 66 vs. 71 years), had more comorbidities (Quan-CCI ≥5, 40% vs. 37%), and more often progressed within 6 months (51% vs, 42%) compared with NHW pts. Similar patterns were seen in the Optum cohort except that NW pts were more likely to be male in the Medicare cohort, but less likely in the Optum cohort.
Chemotherapy was used most common in S1 overall (Medicare: 64%; Optum: 70%) and similar across race/ethnicity (Medicare: 64% in NHW, 66% NW; Optum: 71% NHW, 69% NW). Novel therapy use in S1 was low in both cohorts overall (Medicare, 17%; Optum, 21%) and by race/ethnicity (Medicare: 16% in NHW, 18% NW; Optum: 20% NHW and NW).
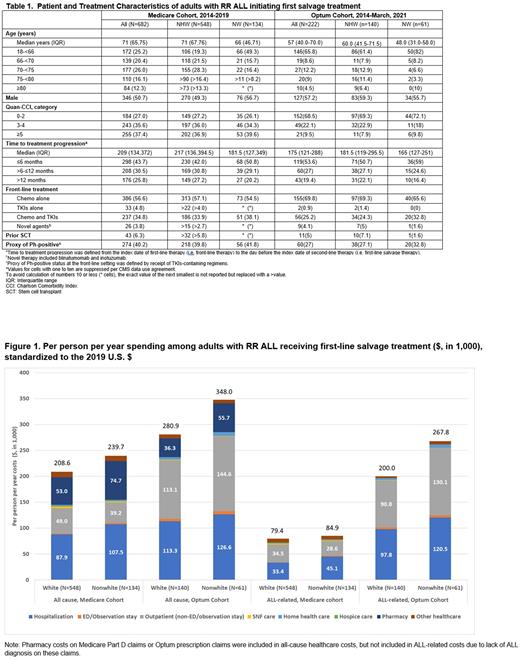
Mean total all-cause and ALL-related costs (PPPY) was higher for NW pts compared with NHW pts for both cohorts (Figure 1). In the Medicare cohort, the largest component of total all-cause costs was inpatient (IP) for both NW (45%) and NHW (42%) while the largest component of total ALL-related costs (not including pharmacy) was IP for NW (53%), but outpatient (OP) for NHW (42%). In the Optum cohort, the largest component of total healthcare costs was IP for NHW (40% all-cause; 49% ALL-related), but OP for NW (42% all-cause; 49% ALL-related).
Conclusions
Findings suggest that in the novel treatment era, novel therapies are not widely utilized in RR ALL pts initiating S1. In a population of insured patients, novel therapy utilization did not vary by race/ethnicity. Variations in cost were observed by race/ethnicity. Findings show NW experienced higher overall costs, which may be driven by the increased comorbidities in NW pts. Additional research is needed to understand the low uptake of novel therapies in RR ALL pts initiating S1 and to characterize specific drivers of cost disparities to inform targeted interventions.
Study limitations include small sample size within the databases analyzed and potential misclassification defining salvage therapy in claims databases.
Disclosures
Braunlin:Amgen: Current Employment, Current equity holder in publicly-traded company. Gong:Amgen: Research Funding. Payne:Amgen: Current Employment. Kou:Amgen: Research Funding. Adedokun:Amgen: Current Employment, Current equity holder in publicly-traded company. Velasco:Amgen: Current Employment, Current equity holder in publicly-traded company. Li:Amgen: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.