Abstract
Peripheral neuropathy is associated with IgM paraproteinemia, with 30-50% of patients with IgM monoclonal gammopathy of undetermined significance (MGUS) and 25% of patients with Waldenström macroglobulinemia (WM) presenting with peripheral neuropathy. IgM-mediated neuropathy is typically a length dependent, bilateral, slowly progressive process that can negatively impact a patient's quality of life and impair activities of daily living. The etiology of the neuropathy can sometimes be clearly linked to antibodies against myelin associated glycoprotein (MAG), amyloidosis, cryoglobulinemia, hyperviscosity, or direct infiltration of the nerves by malignant cells. In many patients, however, the etiology remains unclear and a definitive link to the IgM paraproteinemia remains uncertain. Establishing a definitive etiology is especially challenging in patients with axonal pathophysiology or normal findings on NCS/EMG. Without determining a clear association between the IgM paraprotein and the patient's neuropathy it is difficult to choose the most appropriate treatment. We performed skin punch biopsies on patients with IgM MGUS and WM to evaluate for the presence of monoclonal protein in hopes that this would help reveal the etiology of the neuropathy.
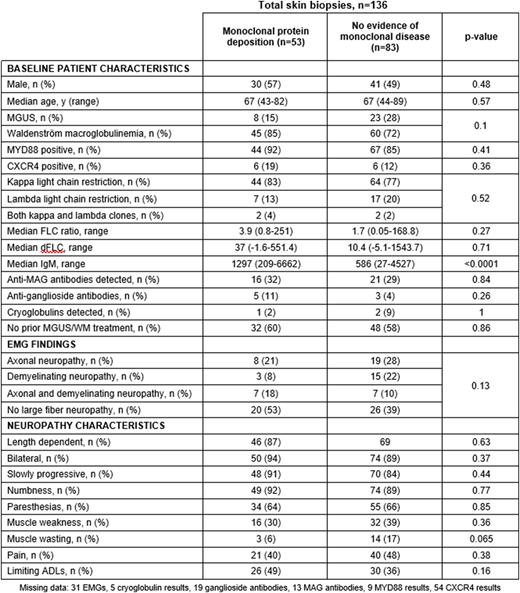
Between January 2020 and June 2022 136 patients (31 with IgM-MGUS, 105 with WM) with symptomatic neuropathy had three full-thickness skin punch biopsies with one specimen from the abdomen and two from the distal lower extremity. Biopsy tissue was evaluated for the presence of monoclonal immunoglobulin, clonal light chains, and amyloid deposition via light microscopy, immunofluorescence microscopy, and electron microscopy. Non-IgM associated causes of neuropathy were also evaluated in each patient. Descriptive statistics were used to evaluate for associations between baseline clinicopathological characteristics. Response outcomes are ongoing and will be updated.
Baseline patient characteristics according to skin biopsy findings are shown in the table. Of the 136 biopsies, 83 patients showed no evidence of malignancy, monoclonal protein, or amyloid deposits in the dermis, blood vessels, or nerves. 53 patients had evidence of monoclonal paraprotein deposition presenting in the following manner: vascular deposition of monoclonal protein (n=17), accumulation of lymphoplasmacytic cells (n=1), monoclonal protein deposition in the dermis (n=12), and monoclonal protein in the nerves (n=27). Additionally, 5 patients were diagnosed with amyloidosis, 2 with Congo red positivity and evidence of amyloid fibrils on electron microscopy and 3 biopsies with fibrillary aggregates consistent with amyloidosis but Congo red negativity. Twenty of the biopsies demonstrating monoclonal IgM deposition were in patients with no evidence of large fiber neuropathy on EMG/NCS. Sixteen of 37 patients with detectable anti-MAG antibodies had findings of monoclonal IgM deposition on biopsy. A higher serum IgM level was seen in patients with monoclonal deposition on biopsies compared with those with negative skin biopsies (p <0.01).
In conclusion, approximately 40% of patients with peripheral neuropathy associated with an IgM MGUS or WM had evidence of monoclonal protein deposition on skin punch biopsies. The association between the monoclonal protein deposition in the skin, nerves, and vasculature and the peripheral neuropathy requires additional investigation and the detection of amyloidosis by skin punch biopsies suggests that this may be used as a potential diagnostic tool for amyloidosis. Skin punch biopsies can be easily performed in the outpatient setting and may represent a novel approach to evaluating peripheral neuropathy in patients with IgM-related disorders.
Disclosures
Sarosiek:ADC Therapeutics: Research Funding; BeiGene: Consultancy. Rennke:Wolters Kluwer: Other: Book authorship; Ionis Pharmaceutical: Consultancy. Doughty:AstraZeneca: Research Funding; Dysimmune Diseases Foundation: Membership on an entity's Board of Directors or advisory committees; Oakstone Publishing: Other: education - CME; Haymarket CME: Other: education - CME; Adler, Cohen, Harvey, Wakeman & Guekguezian LLP: Consultancy. Branagan:CSL Behring: Consultancy; Adaptive Biotechnologies: Consultancy; Genzyme: Consultancy; Janssen/Pharmacyclics: Consultancy; BeiGene: Consultancy; Karyopharm Therapeutics: Consultancy. Treon:BMS: Research Funding; BeiGene: Consultancy; Janssen/Pharmacyclics: Consultancy, Research Funding; X4: Consultancy, Research Funding; Abbvie: Consultancy. Castillo:AstraZeneca: Research Funding; Roche: Consultancy; TG Therapeutics: Research Funding; Pharmacyclics: Consultancy, Research Funding; Cellectar: Consultancy; Beigene: Consultancy, Research Funding; Janssen: Consultancy; Abbvie: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.