Abstract
Introduction: Patients with sickle cell disease (SCD) have vasculopathy due to vaso-occlusion and chronic hemolysis which leads to acute and chronic organ dysfunction and early mortality. Other chronic diseases that may contribute to vasculopathy, such as type 2 diabetes mellitus (T2DM), are becoming increasingly recognized in adults with SCD (PMID 30714090). Following the hemoglobin a1c to assess T2DM control is not recommended in patients with SCD due to the shortened red blood cell life span (PMID 34537047) limiting our ability to monitor glycemic control and its impact on organ function in this patient population. In the general population, poor glycemic control in people with T2DM accelerates kidney dysfunction (PMID 23302714). Risk factors for T2DM and the impact of poor glucose control on kidney dysfunction in SCD are unclear.
Methods: The purpose of this study was to analyze risk factors for T2DM and the effects of glycemic control on kidney function in 439 adult patients with SCD. T2DM was defined by a diagnostic code of diabetes in the electronic health record plus either use of an outpatient antidiabetic agent or serum fructosamine concentration >285mmol/L. The estimated glomerular filtration (eGFR) slope was calculated by linear regression of CKD-EPI 2021-derived eGFR by time per patient. Hyperglycemia was defined as random serum glucose levels >200mg/dL. Statistical testing of cohort characteristics by T2DM status were performed using the Kruskall-Wallis method for continuous variables and Fisher's exact test for categorical variables. Multivariate regression analyses adjusted for age, sex, SCD genotype, systolic blood pressure, body mass index, hydroxyurea use, angiotensin converting enzyme inhibitors (ACEI)/angiotensin receptor blocker (ARB) use, and initial eGFR as covariates.
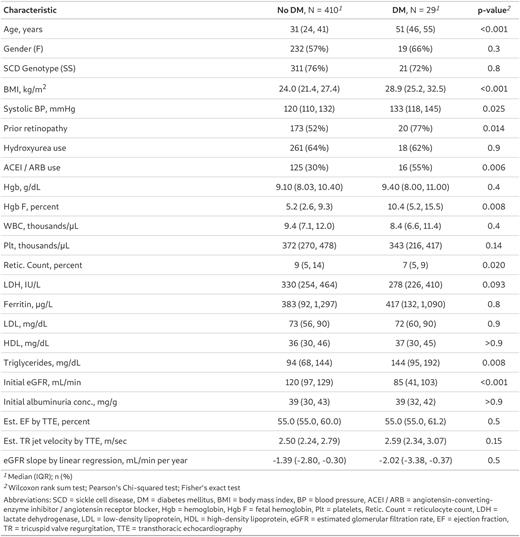
Results: The median age of the cohort was 32 years (interquartile range [IQR], 25-43 years), 57% were female, 76% had hemoglobin SS, and 46% were on hydroxyurea. Twenty-nine (6.6%) had T2DM. Differences in baseline characteristics by T2DM status are provided in Table 1. On logistic regression analysis, older age (OR 1.11; P<0.001), higher body mass index (OR 1.13, P=0.02), and higher serum triglyceride levels (OR 1.01; P=0.02) were independently associated with T2DM.
Within the T2DM group, treatment regimens were heterogenous. Of the 29 patients, 15 (52%) received insulin, 10 (34%) received metformin, 6 (21%) received GLP-1 agonists/DPP-4 inhibitors, 4 (14%) received SGLT-2 inhibitors, and 3 (10%) received alpha glucosidase inhibitors or thiazolidinediones. The median proportion of random blood glucose values in the hyperglycemic range in this SCD cohort was 6.8% (IQR, 0.9% - 14.1% ). We found no strong correlation between fructosamine levels and 14-day glucose averages in time-matched pairs (r2 0.014; P= 0.17). Being on a greater number of antidiabetic medications was associated with a higher risk of hyperglycemia (β 0.058; P=0.008) and average serum glucose (β 18.59; P=0.001).
With a median follow up of 6.7 years (IQR, 3.4 - 8.8 years) the median annual rate of eGFR decline in our cohort was -1.40 (IQR, -2.88 to -0.30) mL/min/1.73m2. We did not observe a difference in the rate of eGFR decline by T2DM status. Interestingly, among the SCD patients with T2DM, the proportion of random blood sugars that were hyperglycemic was independently associated with accelerated eGFR decline (β -5.66; P=0.05) in our fully adjusted model.
Conclusions: Our findings demonstrate that T2DM is relatively common and associated with older age, higher BMI and serum triglyceride levels in adults with SCD. Furthermore, SCD patients with poor T2DM control, as assessed by hyperglycemia, had a more rapid rate of eGFR decline on longitudinal follow up. Our results highlight the need to closely monitor metabolic health indicators, such as elevated BMI, lipid profile and glucose values, to identify patients with SCD at risk for T2DM. Furthermore, strategies to monitor and treat T2DM are urgently needed and may prevent vasculopathy-related complications, such as kidney disease.
Disclosures
Gordeuk:GSK: Consultancy; GBT: Consultancy, Research Funding; CSL Behring: Consultancy, Research Funding; Forma: Consultancy. Saraf:Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Agios: Consultancy; Global Blood Therapeutics: Consultancy, Research Funding, Speakers Bureau; FORMA Therapeutics: Consultancy, Research Funding; ORIC: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.