Abstract
Background: Venous thromboembolism (VTE) is a leading cause of mortality among hospitalized patients, but appropriate thromboprophylaxis remains underutilized. A significant proportion of VTE associated with hospitalization occurs after discharge. We conducted a national survey of healthcare providers to explore attitudes, practices, and barriers related to thromboprophylaxis in hospitalized patients, including practices for post discharge VTE prevention.
Methods: We developed a survey exploring current attitudes and practices around VTE prophylaxis in adult hospitalized patients. Healthcare providers targeted for the survey were physicians, nurses, physician assistants, and pharmacists. The survey was administered to a targeted convenience sample. Participants were recruited through social media, professional healthcare organizations, and internal medicine program directors across the US. The overarching survey areas included (1) use of appropriate prophylaxis, including perceived rates of appropriate prophylaxis at respective institutions, (2) perceived barriers to appropriate prophylaxis, (3) practices to educate about and prevent post discharge VTE events, and (4) views on use of risk assessment models (RAMs) and other strategies to improve rates of VTE prophylaxis. Since it is generally understood by the healthcare provider respondents of this survey that administration of VTE prophylaxis depends on a patient's risk, survey questions did not specify a definition for appropriate prophylaxis. We summarized data as proportions with 95% confidence intervals (CI).
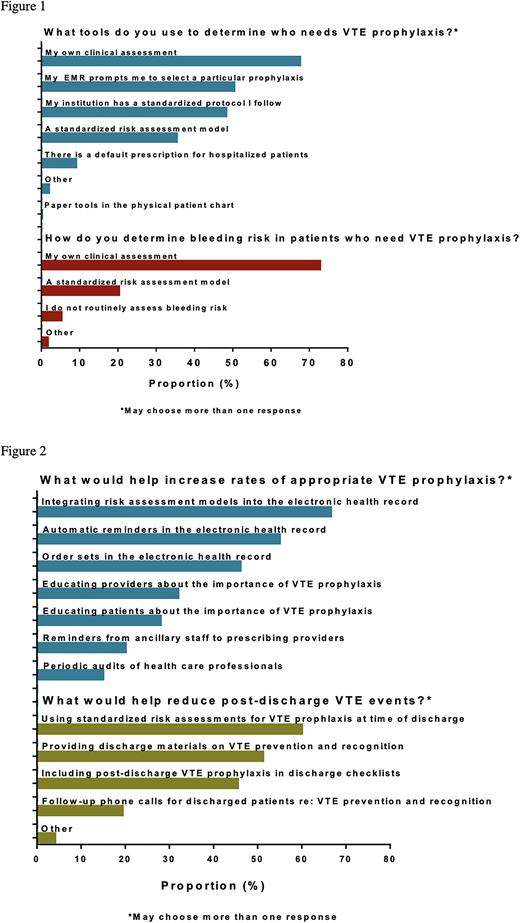
Results: Of 607 U.S.-based respondents, 69.9% were 40 years or younger, 55.7% were female, 68.2% were white, and 63.1% reported working in an academic hospital. Physicians comprised 70.7% of respondents, of whom 46.6% identified as trainees; among non-trainees, 49.0% had been in practice for more than 10 years. Hospital medicine was the most frequent specialty (52.1%) followed by hematology (20.8%). Nearly all respondents agreed that VTE prophylaxis is important for patient care (98.8%, 95% CI: 97.6-99.5) and that current measures are safe (92.6%, 95% CI: 90.2-94.5) and effective (93.8%, 95% CI: 91.6-95.6). Yet only 52.0% (95% CI: 47.9-56.0) of respondents perceived that hospitalized patients at their institution were on appropriate VTE prophylaxis almost all of the time. The most commonly cited reasons for patients not being on appropriate VTE prophylaxis included patient refusal (21.8%), risk of bleeding outweighs benefit (21.6%), and unclear indications (16.0%) and contraindications (17.6%) for prophylaxis. Less than half of respondents reported using institutional protocols (48.3%) or a standardized RAM (35.4%) to select patients for VTE prophylaxis and most respondents (72.3%) relied on clinical judgement to assess bleeding risk when deciding on prophylaxis (Figure 1). Respondent views on strategies that could improve VTE prophylaxis rates in hospitalized patients included integration of RAMs into electronic health records (66.6%), automatic electronic reminders (55.0%), and order sets in electronic systems (46.1%) (Figure 2). Less than 20% of respondents reported routinely educating patients about risks (15.1%, 95% CI: 12.3-18.2) and symptoms (17.9%, 95% CI: 14.9-21.2) of post-discharge VTE events, and 8.6% (95% CI: 0.06-11.1) routinely prescribe VTE prophylaxis on discharge. Respondent views on strategies that could help reduce post-discharge VTE events included using standardized risk assessments at discharge (60.0%), providing educational materials at discharge (51.2%), and including post-discharge VTE prophylaxis in discharge checklists (45.5%) (Figure 2).
Conclusion: To our knowledge, this is the largest U.S. national survey to date that focuses on VTE prevention practices in hospitalized patients. VTE prophylaxis was almost universally accepted as important, safe, and effective for patients at risk for VTE. Less than half of the respondents reported using standardized protocols or RAMs to guide appropriate thromboprophylaxis administration. Discharge education regarding risks of VTE is infrequent. This national multidisciplinary survey study highlights gaps in current practices and strategies for VTE prevention in hospitalized patients.
Disclosures
Rosovsky:Janssen: Consultancy; abbott: Consultancy; BMS: Consultancy; Inari: Consultancy; Penumbra: Consultancy; dova: Consultancy. Zwicker:Quercegen: Research Funding; Parexel: Consultancy; Pfizer/BMS: Honoraria; Portola: Honoraria; CSL: Consultancy; Sanofi: Consultancy; Incyte: Research Funding; Daiichi: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.