Abstract
Introduction Expected graft-versus-leukemia (GVL) effect, allogeneic hematopoietic stem cell transplantation (allo-HCT) is performed for myeloid malignancies. GVL is modulated by alloreactive T cells that recognize cancer cell antigens, but not all the mechanisms of GVL have been elucidated. Alloreactive T cells can also cause a harmful immune response, graft-versus-host disease (GVHD).
Human leukocyte antigens (HLA) are the key molecules presenting antigens to T cells. They are highly polymorphic and vary widely among individuals. HLA allelic diversity causes differences in the immunopeptidome breadth. Recent reports suggest that a smaller immunopeptidome breadth may result in autoimmune disease such as aplastic anemia or type I diabetes, and that larger differences may enhance the antitumor effects of immune checkpoint inhibitors.
This suggests that understanding the impact of the HLA immunopeptidome on allo-HCT, which may also be relevant to GVL and GVHD, might improve outcomes.
Aim To examine the association between HLA class I immunopeptide diversity and outcomes in patients undergoing allo-HCT.
Methods From 2006 to 2021, 145 patients with myeloid malignancies underwent initial allo-HCT at our institution. Of the 109 patients with evaluable allele data, 53 who received 8/8 allele-matched donors (acute myeloid leukemia, n = 40; myelodysplastic syndrome, n = 13) were analyzed. Graft sources were bone marrow (n = 31) and peripheral blood stem cells (n = 23). Donors were related (n = 23) and unrelated (n = 30). The conditioning regimens were myeloablative (n = 31) and non-myeloablative (n = 21). The disease status pre-transplantation was standard risk (n = 30) and advanced stage (n = 23).
Differences in the immunopeptidome breadth between individuals were quantified as HLA evolutionary divergence (HED). HED was calculated using Grantham distance, which predicts amino acids from HLA allelic information and attempts to measure evolutionary distance based on the chemistry of the two amino acids. HLA allele data were drawn from clinical records and analyzed in the HLA laboratory (Kyoto, Japan) or SRL, Inc. (Japan). The calculator program was produced by Tobias Lenz et al. (https://hladiv.net/). The HED of each HLA class I: HLA-A, HLA-B, and HLA-C was calculated. Based on HED degree, overall survival (OS), cumulative relapse rate (CIR), acute/chronic GVHD, and non-relapse mortality (NRM) were evaluated.
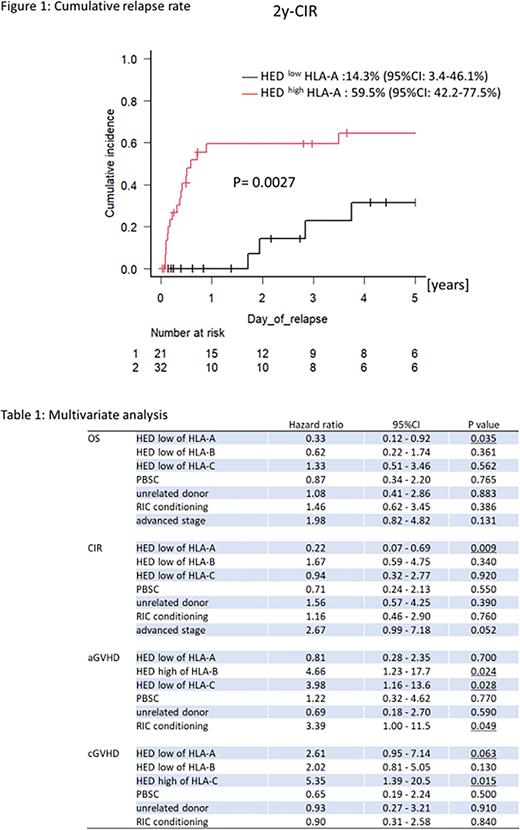
Result The median HED (range) was HLA-A, 10.34 (0.00-13.70); HLA-B, 7.50 (0.00-14.33); and HLA-C 4.66, (0.00-7.60), respectively. Based on their median HED, patients were divided into HED high or HED low groups for HLA-A, HLA-B, and HLA-C.
On univariate analysis, patients with HED low for HLA-A had better 2-year OS compared to HED high for HLA-A (80.4%; 95%CI, 55.6%-92.2% vs. 42.0%; 95%CI, 23.9%-59.1%; p = 0.025) and better 2-year CIR (14.3%; 95%CI, 3.4%-46.1% vs. 59.5%, 42.2%-77.5%; p = 0.0027) (Figure 1). HED levels of HLA-B and HLA-C were not related to OS (p = 0.501, and p = 0.972, respectively) or CIR (p = 0.257 and 0.796, respectively). NRM was not associated with HED levels for any of the HLA. Multivariate analysis found HED low for HLA-A to be a favorable risk factor for OS (HR, 0.46; 95%CI, 0.22-0.95; p = 0.035) and CIR (HR, 0.22; 95%CI, 0.07-0.69; p = 0.0092) when adjusted for HLA-B, HLA-C, donor, graft, conditioning, and disease status.
Next, the association between the HED level of each HLA class I and GVHD was analyzed. In acute GVHD, grades 2-4, after adjusting for graft, donor, and conditioning, HED high of HLA-B (HR, 4.66; 95%CI, 1.23-17.7; p = 0.024) and HED low of HLA-C (HR, 3.98; 95%CI, 1.16-13.6; p = 0.028) were risk factors but not for HLA-A. In chronic GVHD, multivariate analysis found HED high for HLA-C was a risk factor (HR, 4.77; 95%CI, 1.13-20.2; p = 0.034). Also, HED low for HLA-A tended to increase chronic GVHD ((HR, 2.61; 95%CI, 0.95-7.14; p = 0.063) (Table 1).
Conclusion HED low for HLA-A was a favorable risk factor for OS and CIR, possibly because chronic GVHD tended to increase with HED low of HLA-A. HED levels for HLA-B and HLA-C did not contribute to OS and CIR but did influence acute and chronic GVHD. Since immunopeptidome significance may differ for each HLA class I, consideration of HED level during the donor selection may improve the safety and efficacy of allo-HCT.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.