Abstract
Background Antiphospholipid syndrome (APS) is a highly prothrombotic acquired autoimmune disease characterised by thrombosis and/or pregnancy morbidity with the persistent presence of antiphospholipid antibodies (aPL).Anticoagulation is the mainstay of treatment for APS however risk of recurrence remains high especially in triple antibody positive patients. Recent clinical studies demonstrated that DOACs are not as effective as Vitamin K Antagonists (VKA) in patients with APS especially those who are triple positive. However, the use of DOACs in patients without triple positive aPL remains variable.
Aims 1)To assess real-life anticoagulation practice in the UK
2)To assess the rates of recurrent thrombosis, major bleeding and minor bleeding (as per International Society of Thrombosis and Haemostasis) in patients with thrombotic APS
Methods This was a multicentre observational study. Data was collected using a pre-designed standardised case record form via a secure online data entry platform (REDCap). Only patients age ≥18 years with confirmed diagnosis of APS were included in the study.
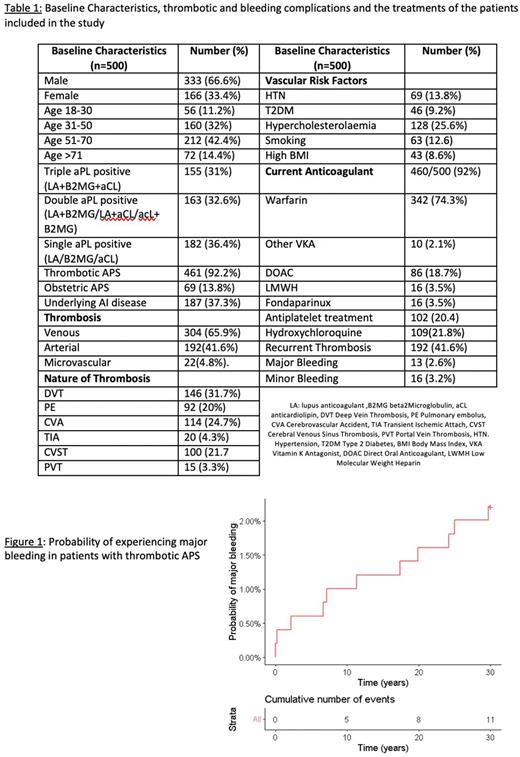
Results The study included 500 patients with APS from 15 National Health Service (NHS) Trusts across the UK. The mean age was 52.9 (-/+ 15.94) years and 66.6% (333/500) were male. Frequency of single, double, and triple positivity for aPL were 36.4%, 32.6% and 31% respectively. Almost 40% of patients (37.3% , 187/500) had underlying autoimmune disease in addition to APS. Of the 500 patients, 92.2% (461/500) had at least one thrombotic event, 13.8% (69/500) had obstetric complications and 4.6% (23/500) had both thrombotic and obstetric complications. In patients with thrombotic APS, venous thrombosis occurred in 65.9% (304/461) patients, arterial thrombosis in 41.6% (192/461), and microvascular thrombosis in 4.8% (22/461) respectively.
Almost all patients (99.8%; 460/461) with a thrombotic history were on anticoagulants (460/461). Of these 76.5% (352/460) were on VKAs whilst only 18.7% (86/460) were on DOACs. The rest of the patients were on low molecular weight heparin (3.5%) and fondaparinux (1.3%). Of the 342 patients on warfarin 207 patients 61% (207/342) had an INR target of 2.5 (2.0-3.0) , 10.5% (36/342) had a target of 3.0 (2.5-3.5) and 28.9% (99/343) had target INR of 4.0 (3.5-4.5). Additionally, 29.8% (102/342) of patients on anticoagulation were on antiplatelet treatment and 31.9% (109/342) patients were on Hydroxychloroquine (HCQ).
Of the 155 patients with triple positive APS, 64.5% (100/155) were on warfarin and 20.6% (32/500) were on DOACs and the remainder on LMWH or fondaparinux. In those with arterial thrombosis, the vast majority were on warfarin 82.8% (159/192) with 5.2% (10/192) on a DOAC and a small minority on LMWH or fondaparinux. Of the 192 patients with arterial thrombus, 68 (19.8%) were triple positive aPL and of these 7.4% (5/68) were on a DOAC. Table 1 shows the baseline characteristics of the study group.
Recurrence of thrombosis occurred in 41.6% (192/461), most frequently within 3 years of diagnosis (65.1%, 125/192). The frequency of major (Figure 1) and minor bleeding were 2.8% (13/461) and 3.2% (16/461) respectively.
Dual or triple aPL status, smoking, hypertension, and ischaemic heart disease were significantly associated with recurrent thrombosis on univariate but not multivariate analysis, confirming a multifactorial contribution for thrombosis.
In both univariate and multivariate analysis, increasing age was significantly associated with major bleeding [hazard ratio (HR) 1·05, 95% confidence interval (CI) 1.01-1·10; P = 0·022]. Notably, a higher target INR was associated with major bleeding.
Conclusions In the largest UK study of APS to date we assessed anticoagulation practice, recurrent thrombosis rate and bleeding rate in this cohort. The frequency of recurrence of thrombosis in APS was as high as 41.6% (192/461) with most patients developing recurrence within the first 3 years of diagnosis. Frequency of major and minor bleeding were 2.8% (13/461) and 3.2% (16/461) respectively. Age was a significant contributor for major bleeding whilst thrombosis was multifactorial. Although VKA remains the main anticoagulant of use in patients with thrombotic APS, there are wide variations in the practice within the UK which are mostly, but not wholly, adherent to national guidelines especially in the context of triple positive thrombotic disease and arterial thrombosis.
Disclosures
Crossette-Thambiah:Roche: Honoraria. Breen:Bayer: Honoraria; Veniti: Honoraria. Laffan:Silence Therapeutics: Consultancy. Jayakody Arachchillage:Takeda: Honoraria; Bayer, Leo Pharma: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.