Abstract
Background: Venous Thromboembolism (VTE) affects morbility of Hodgkin Lymphoma (HL) patients. Thrombosis Lymphoma (ThroLy) and Khorana scores have been conceived to predict the basal thrombotic risk in patients with lymphoma and cancer, respectively. Currently, there is no univocal indication to perform thrombosis prophylaxis in HL, mostly guided by clinical judgement.
Methods: We performed a retrospective study to validate these scores on a cohort of HL and to evaluate other potential risk factors for thrombosis. Consecutive patients with newly diagnosed HL from 2018 to 2020 were included. Hematological features and major comorbidities were included in the analysis. Statistical analysis was performed with univariate analysis (χ2-test; Kaplan-Meier curve) and multivariate analysis (COX-regression model).
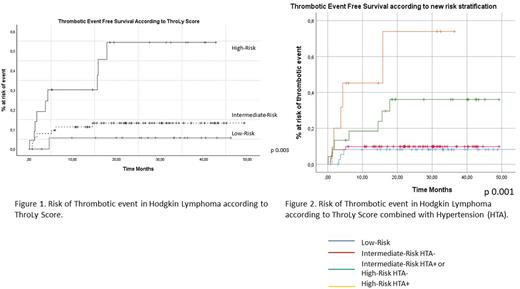
Results: We evaluated 166 patients, with a median age at diagnosis of 42.5 years (range 18-85), and a median follow-up of 27.7 months (range 6-54). According to Khorana criteria, intermediate-risk (IR) patients were 81.9% (n=136), while high-risk (HR) were 18.1% (n=30). Regarding ThroLy criteria, low-risk (LR) patients were 27.1% (n=45), IR were 52.4% (n=87) and HR were 20.5% (n=34). All patients received first-line therapy (99% ABVD regimen), and 22 (13.6%) subsequently experienced a relapse/progression. Peripherically implanted central catheter (PICC) was implanted in 51.2% (n=85). No patient had a previous history of thrombosis. A subgroup of patients, 15.7% (n=26), received enoxaparine as thrombosis prophylaxis for bulky or mediastinal disease, and was excluded from thrombotic scores validation. A total of 21 thrombotic events were observed in 140 (15.1%) patients after a median time from diagnosis of 2.8 months (range 0.17-18.8); only 2 were arterial. At univariate analysis, 13 events were PICC-related (PICC 19.1% versus no PICC 11.3%, p 0.15); according to age, patients above 60 years at diagnosis showed higher rate of thrombotic events, 23.3% (7/30) versus 12.8% (14/109) for patients below 60 years (p 0.15). Patients with Bulky disease not performing prophylaxis presented higher incidence of events (28% 7/25 vs 12.3% 14/115, p 0.05) Khorana HR group showed a trend of increased events rate compared to IR, 28.6% (6/24) vs 12.9% (15/116) respectively (p 0.09). Robust association was found between ThroLy risk categories and thrombotic risk: among HR patients, VTE was observed in 37.5% (9/24) versus 12.2% (9/75) and 7.3% (3/41), for IR and LR respectively, with an estimated thrombotic event-free survival (EFS) of 30 months for HR versus 51 for LR (p 0.003, Figure I). No significant association was found related to sex (p 0.72), GHSG classification (p 0.301), histology subtype, Disease Stage (p 0.97), post-chemotherapy neutropenia (p 0.397), bone marrow involvement (p 0.88), diabetes (p 0.62), response to treatment (p 0.15) and erythropoietin employment (p 0.78). Even continuous variables such as WBC, Hb, platelets, ESR did not differ significantly in relationship to thrombotic risk. HR ThroLy (HR 2.81, p 0.009 CI 1.2-6) was identified as independent risk factor on multivariate analysis. Among evaluated risk factors, hypertension (HTA) requiring treatment showed a significant association to thrombotic events: among hypertensive patients a higher rate of VTE was observed with 27.6% (8/29) opposed to 11.8% (13/111) in non-hypertensive patients (OR 1.32 range 0.94-1.87, p 0.04). We then defined new risk categories combining HTA and ThroLy score: 1) HR ThroLy patients with HTA, thrombotic events in 45.5% (5/11); 2) HR without HTA (30.8%, 4/13) and IR with HTA (28%, 3/11), thrombotic events in 29.6% (7/24); 3) IR without HTA, thrombotic events in 9.4% (n=6/64) not different from 4) LR, thrombotic events 7.5% (3/40) (Figure II, p 0.001).
Conclusion: ThroLy score proved its utility in VTE-risk assessment in HL; HTA could be integrated to augment ThroLy predictive power in discriminating super HR patients, who might be eligible to anti-thrombotic prophylaxis.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.