Abstract
Background:
Five-year overall survival for patients with myelodysplastic syndromes (MDS) is around 30%. Adverse prognostic factors include advancing age, higher blast cell percentage, poor risk cytogenetics, two or more cytopenias, high burden of comorbidity, and transfusion-dependency. The impact of socioeconomic position on clinical outcomes in MDS patients is however unclear. In this nationwide population-based cohort-study, we therefore examined the associations between the individual-level socioeconomic markers education level, cohabitation status, and income, and the risk of progression to acute myeloid leukemia (AML), and all-cause mortality among MDS patients.
Methods:
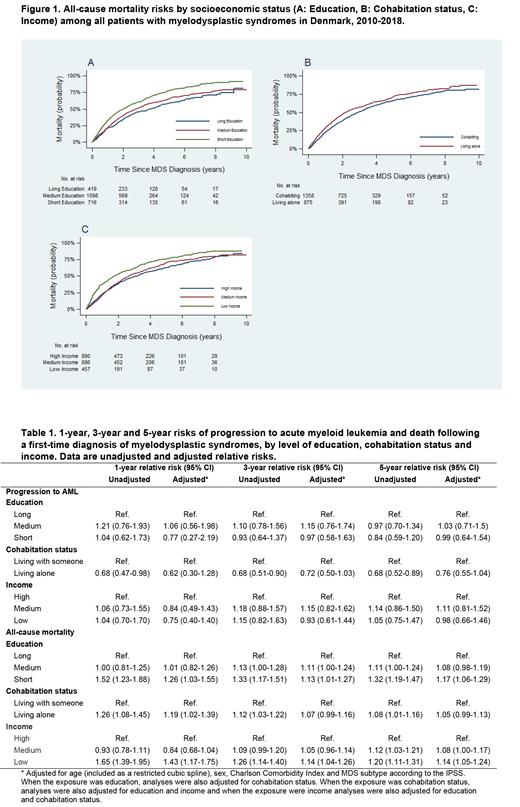
Using the Danish Myelodysplastic Syndromes Database, we identified all patients with incident MDS diagnosed between January 1st 2010 and December 31th 2018. The database holds valid and detailed patient- and disease-characteristics on all Danish MDS patients diagnosed since 2010. We linked the study-population with individual-level information on education, cohabitation status, income, comorbidity, progression to AML, and vital status retrieved from high-quality Danish population-based registries. We computed absolute risks of progression to AML and all-cause mortality using the cumulative incidence (risk) function accounting for death as competing risk when AML was the outcome. Also, 1-year, 3-year, and 5-year relative risks (RRs) of progression to AML and death were computed using the pseudovalue approach. All results were given crude and adjusted for age, sex, socioeconomic position (SEP), comorbidity and subtype of MDS according to the "International Prognostic Scoring System" (IPSS) and with 95% confidence intervals (CIs).
Results:
The final cohort comprised 2233 MDS patients (median age 75 years, 63% males). Median follow-up time was 1.7 years. The 1-year risks of progression to AML was similar across education levels (long education (>13 years): 5%, medium education (9-12 years): 6%, short education (<9 years): 6%. In adjusted models, there were no associations between education, income or cohabitation status and risk of progression to AML (Table 1). Still, patients with a short education had higher 1-year all-cause mortality (33%) compared to those with medium (22%) and longer education (21%) (Figure 1). In adjusted models the risk of death one year from diagnosis was higher in patients with short vs. longer education [RR=1.26 (95% CI: 1.03-1.55)], in patients with lower vs. higher income [RR=1.43 (95% CI: 1.17-1.75)], and among patients who were living alone compared to those who lived with someone [RR=1.19 (1.02-1.39)]. The increased risk of death among patients with short education, low income, and those who lived alone persisted after 3-year and 5-years of follow-up (Table 1).
Conclusion:
In a real world setting, shorter education, living alone, and lower income were not associated with increased risk of progression to AML but with inferior survival in Danish MDS patients. These results suggest that in spite of "free and equal access" to healthcare and cancer treatment in Denmark, short education, living alone, and low income are adverse prognostic factors for patients with MDS. Further analyses are ongoing to get insight into the mechanisms driving these socioeconomic disparities in MDS patients.
No relevant conflicts of interest to declare.