Abstract
Introduction: Primary myelofibrosis (PMF) is a chronic myeloproliferative neoplasm characterized by cytopenias, splenomegaly and a risk of leukemic transformation. In light of newer therapies such as ruxolitinib that are not curative but can improve quality of life, the timing of transplant needs more in-depth analysis to determine which patients would benefit from an early versus delayed transplant strategy.
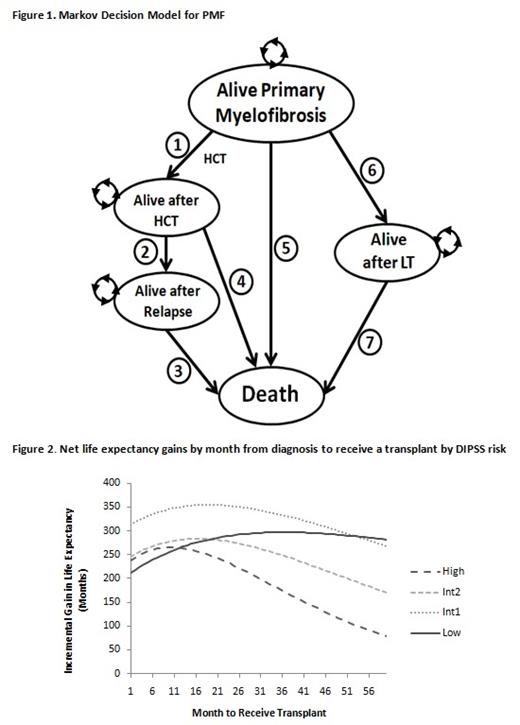
Methods: We developed a Markov cohort model to simulate the long-term disease trajectory in patients with PMF and predict the optimal timing of transplant stratified by a Dynamic International Prognostic Scoring System (DIPSS) risk. Our model consisted of five health states including alive with PMF, alive after leukemic transformation, alive after transplant, alive after relapse and death. Transition probabilities between health states were acquired from published literature on the natural history of the disease and outcomes following transplantation. The model was run over a patient's lifetime until all patients transitioned to the death state. We used a cycle length of one-month to represent the natural progression of PMF. The structure of the Markov model is delineated in Figure 1. In this decision model, a hypothetical cohort of patients begins in the Alive-PMF state and can transition after each monthly cycle to other health states. Patients could remain in an alive state for any number of cycles without transitioning to another health state, indicated by the arrow wheels. We performed probabilistic analyses by jointly varying all model parameters over 1000 simulations and calculated 95% confidence intervals (CI) for the model outcome.
Results: Regardless of DIPSS risk, all patients with PMF benefited from a transplant with respect to life expectancy gained (Figure 2). Life expectancy gains from a transplant among patients with high-risk disease peak at 9.7 months (95% CI: 9.5-9.9) from diagnosis, while patients with intermediate-2 disease have a peak gain in life expectancy at 16.6 months (95% CI: 16.4-16.8). Intermediate-1 DIPSS risk patients have a more delayed time frame where the net gain in life expectancy from transplant begins to slow at 20.5 months (95% CI: 20.2-20.7). Patients with low risk DIPSS had greater net gain in life expectancy the longer transplant was delayed; this trend plateaued at 29 to 45 months, when thereafter net gain in life expectancy begins to be lost (Figure 1).
Conclusion: Our modeling suggests that transplant processes including donor selection and pre-transplant work-up are indicated upfront for patients diagnosed with intermediate-2 and high risk PMF, while this can be delayed for patients with low or intermediate-1 risk disease. This model should provide clinicians with guidance on when to refer eligible patients with PMF for transplantation.
Kekre: Novartis: Consultancy, Honoraria; Gilead: Consultancy, Honoraria; Celgene: Consultancy, Honoraria.