Abstract
Background
Primary mediastinal large B-cell lymphoma (PMBCL) is a rare disease with the majority of patients being rapidly progressive anterior mediastinal large tumors. Due to the rarity of PMBCL, information on the incidence, clinical features, prognostic factors and models of PMBCL is limited. The present study is one of the largest studies on the incidence and prognostic factors of PMBCL and is the first to establish a nomogram model of PMBCL and validate it with real-world data. We also compared the newly established Nomogram with the existing IPI prognostic model. We believe that our findings can help clinicians to quickly and accurately assess the predicted survival of patients and help them to perform individualized risk stratification of patients.
Methods
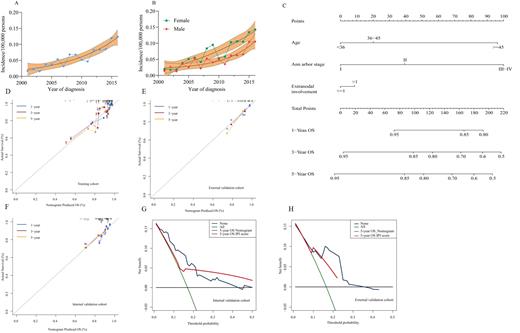
Based on data from the Surveillance, Epidemiology and End Results (SEER) database, 797 patients diagnosed with PMBCL were enrolled in this study. The 797 patients were randomly divided into training and internal validation groups in a 7:3 ratio, and 116 patients diagnosed with PMBCL were included in the external validation group based on data from the Sun Yat-sen University Cancer Center and the First Affiliated Hospital of Guangzhou Medical University. Independent prognostic factors were screened by Cox regression analysis. R-coding was used to construct nomograms predicting overall survival (OS). Discriminations and corrections of the new model were assessed using the consistency index (C-index), subject operating characteristic curves (ROC) and calibration curves, and compared with the conventional international prognostic index (IPI) using decision curve analysis (DCA) to assess its accuracy and benefit.
Results
From 2001 to 2016, the incidence of primary mediastinal large B-cell lymphoma showed a relatively stable increasing trend with an APC of 11.8% (95% confidence interval 8.8-14.0, P<0.05), and this trend was more pronounced in the female population. Multivariate models showed that age and Ann arbor staging were significantly associated with OS, while the variable of extra-nodal invasion was included in the modeling based on clinical experience. In the training cohort, the C-index of the nomogram for OS was 0.712. the C-index for the internal and external validation cohorts was 0.667 and 0.690, respectively. The calibration curve also showed high predictive accuracy. The C-index and ROC curves of nomogram showed better results compared to IPI scores, and also yielded better net gains in decision curve analysis.
Conclusion
In summary, we successfully established a validated nomogram for predicting OS in patients with PMBCL, which can help clinicians to select appropriate individualized treatment for their patients.
No relevant conflicts of interest to declare.