Abstract
Background
Large granular lymphocyte leukemia associated pure red cell aplasia (LGLL-PRCA) accounts for a significant portion of secondary PRCA. Cyclosporine (CsA) and cyclophosphamide (CTX) are the main immunosuppressive agents used in treating LGLL-PRCA [1]. Considering the cytotoxicity of CTX, CsA may be proposed as first-line therapy [2]. However, because of the rarity of LGLL-PRCA, long-term responses and relapse rates after CsA and CTX therapy are largely unknown.
Methods and results
From September 2009 to December 2020, we selected 65 uniformly diagnosed LGLL-PRCA and analyzed clinical features and treatment outcomes of CsA and CTX.
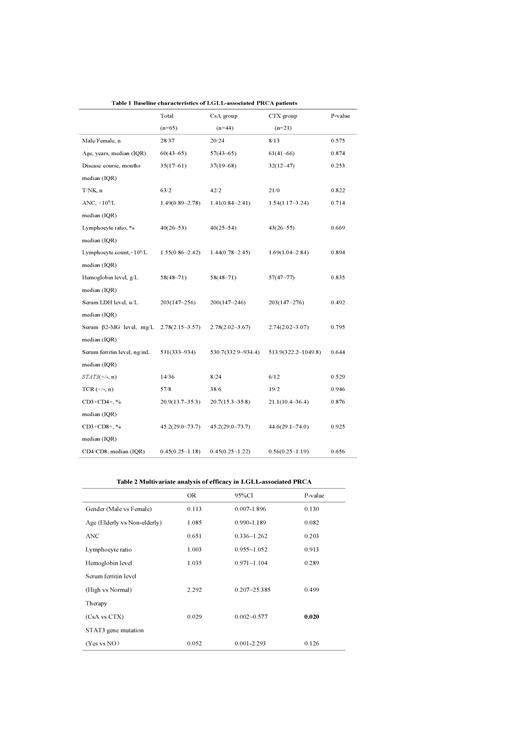
In the present study, 43.1% harbored neutropenia (<1.5×10 9/L) and only 1 patient had spondyloarthritis (Table 1). Besides, we found that 9.2% developed recurrent oral ulcer and 18.5% had reduced serum complemet C3 level, both of which were related to abnormal immune status.
In our cohort, 44 patients received CsA therapy and 21 patients received CTX therapy. 53.8% (35/65) obtained erythroid lineage response and 26.2% (17/65) achieved complete response. CTX produced higher response rate (81.0% vs 40.9%, P=0.002) and complete response rate (47.6% vs 15.9%, P=0.007) than CsA. We further analyzed related factors influencing efficacy by Binary-Logistic multivariate regression model and found that higher response rate was mainly related to CTX therapy (P=0.02) (Table 2).
We detected STAT3 and STAT5b gene in 50 cases. None of the patients had STAT5b mutation and 14 patients had STAT3 mutation. 12 of 14 mutation cases were non-elderly patients (<60 years ). For younger patients, STAT3 mutation was more frequent (85.7% vs 22.2%, P<0.01). In STAT3 mutation group, patients appeared to respond better to CTX than CsA (83.3% vs 37.5%, P=0.138).
Up to the last follow-up, 11 patients treated with CsA recurred after CsA reduction or discontinuation, with a median relapse time of 10 (3~80) months after remission. Only 1 patient relpsed after the discontinuation of CTX due to neutropenia and returned to remission status after CTX retreatment. In our research, CsA had higher recurrence rate than CTX without statistical significance (25.0% vs 4.8%, P=0.104).
Discussion
CsA may be proposed as first-line therapy for LGLL-PRCA [2,3]. CTX also appears to be a good treatment choice, but CTX should not be used for more than 12 months since associated toxicities and the risk for developing myelodysplastic syndromes and acute myeloid leukemia. Therefore, it is necessary to compare the efficacy of CsA or CTX in the treatment of LGLL-PRCA.
Deep sequencing analyses of residuals LGLL clones reveals that CTX could eradicate LGLL clones, providing durable response, low relapse rate, whereas CsA is associated with the persistence of leukemic clones, and high frequency of relapse [4]. Our results show that the response rate of CTX is higher than CsA (P=0.02), and the probability of recurrence is relatively low (25.0% vs 4.8%, P=0.104). This is consistent with the results of previous study by Rajala [4].
It was important to note that patients with STAT3 mutations are more likely to respond to MTX [5]. Our study showed that the response rate for CTX was 83.3% in patients with STAT3 mutations, which was seemingly higher than CsA (37.5%), although remained statistically insignificant (P=0.138) that might be due to small number of cases.
Conclusions
The results of the current study may reflect the real world experience of LGLL-PRCA in whom treated by CTX or CsA, may be limited by its retrospective nature, small cohorts. In preliminary conclusion, LGLL-PRCA could acquired better response to CTX than CsA. Besides, CTX may reduce relapse.
References
1. Means RT Jr. Pure red cell aplasia. Blood, 2016, 128(21): 2504~9.
2. Moignet A, Lamy T. Latest Advances in the Diagnosis and Treatment of Large Granular Lymphocytic Leukemia. Am Soc Clin Oncol Educ Book, 2018, 38: 616~25.
3. Go RS, Tefferi A, Li CY, et al. Lymphoproliferative disease of granular T lymphocytes presenting as aplastic anemia. Blood, 2000, 96(10):3644~6.
4. Rajala HLM, Olson T, Clemente MJ, et al. The analysis of clonal diversity and therapy responses using STAT3 mutations as a molecular marker in large granular lymphocytic leukemia. Haematologica, 2015, 100: 91~9.
5. Loughran TP, Zickl L, Olson TL, et al. Immunosuppressive therapy of LGL leukemia: prospective multicenter phase II study by the Eastern Cooperative Oncology Group (E5998). Leukemia, 2015, 29(4): 886~94.
No relevant conflicts of interest to declare.