Introduction
Allogeneic hematopoietic cell transplantation (HCT) remains the sole curative therapy for patients with juvenile myelomonocytic leukemia (JMML) leading to a 5-year disease-free survival of ~50%. Whether donor NK cell determinants (e.g., KIR mismatch, KIR A/B genotype) correlate with relapse and survival are unknown. We previously demonstrated that JMML stem cells, defined as Lin-CD34+CD38-, express ligands for NKG2D, NKp30, and NKp44 at levels equal or greater than AML stem cells and that colony-forming units were significantly reduced following incubation of JMML cells with NK cells. Based on these observations we hypothesized that NK cell-dependent mechanisms are a major component of protection from JMML relapse after HCT, and specifically that determinants of greater donor NK cell function (e.g. KIR Bx donors or KIR ligand mismatch) are associated with reduced relapse. We therefore investigated NK cell-related donor and recipient immunogenetics as determinants for outcomes in children transplanted for JMML.
Methods:
Patients (0 to < 19 years) who received a first allogenic HCT from an alternative donor between 2000 to 2017 and had available donor samples from the Center for International Blood and Marrow Transplant Research (CIBMTR) repository were included in the study. Donor KIR typing was performed on pre-HCT samples and results were correlated with clinical data extracted from the CIBMTR database. The primary endpoint was disease free survival (DFS); secondary endpoints included relapse rate (REL), acute graft versus host disease (aGVHD), chronic graft versus host disease (cGVHD), GVHD relapse free survival (GRFS) and overall survival (OS). Patient and transplant related variables included age (< 2 years vs ≥ 2 years), sex, race, performance score (< 90 vs >90), disease status, graft type (bone marrow, peripheral blood, and cord blood), HLA matching (8/8 vs others), conditioning intensity (myeloablative vs others), use of serotherapy, GVHD prophylaxis (calcineurin inhibitor (CNI)+ methotrexate (Mtx) ± others vs others) and year of HCT (2000-2007 vs 2008-2017). KIR models tested included KIR genotype (AA vs Bx), Donor KIR B content (0-1 vs ≥ 2), centromeric and telomeric region score (AA vs AB vs BB), donor KIR B content score (best, better, neutral), KIR composite score (2 vs 3 vs 4), activating KIR content, presence of activating KIR DS4, ligand-ligand (L-L) mismatch, KIR ligand (KIR-L) mismatch, and missing ligand. Proportional hazards were checked for all covariates in every model. Univariate analysis was performed for primary and secondary outcomes of interest. Covariates with overall p-value < 0.05 and pairwise comparisons with p-value < 0.05 were considered significant. L-L and KIR-L mismatch effects were studied for all outcomes in a subgroup of HLA-mismatched donors (high resolution match <8/8).
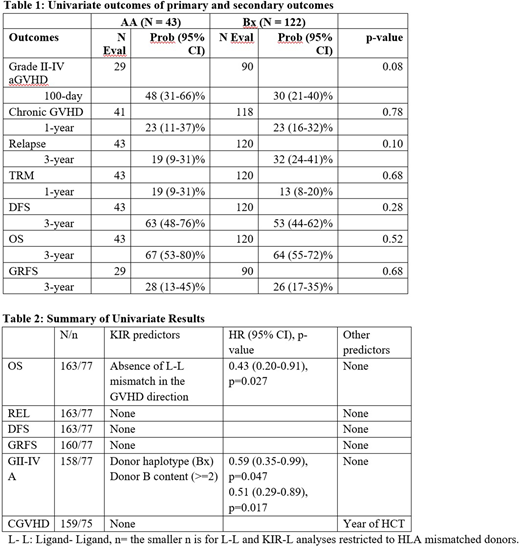
Results: 165 patients (113 males) with a median follow up of 85 (6-216) months met the study criteria. Of these, 111 received an unrelated donor transplant and 54 received cord blood transplants. This included 77 HLA-mismatched donor transplants. Almost all (161, 98%) received myeloablative conditioning. Half of the study cohort received ATG (91, 55%) and CNI + Mtx based GVHD prophylaxis (81, 49%). Based on donor KIR genotype, 43 patients received grafts from AA donors and 122 from Bx donors. On univariate analysis, there was no difference between AA vs Bx for the primary and secondary outcomes (Table 1). Considering the various KIR models, OS was significantly better for patients without L-L mismatch in the GVHD direction (HR 0.43 (95% CI: 0.20-0.91), p=0.027). Risk of grade II-IV aGVHD was lower in patients with Bx donors (HR 0.59 (CI: 0.35-0.99), p=0.047) and donors with B content score of ≥ 2 (HR 0.51 (0.29-0.89), p=0.017) (Table 2).
Conclusion: To our knowledge this is the first study analyzing NK determinants in pediatric JMML HCT recipients. OS and aGVHD were the only outcomes associated with NK cell immunogenetics, but not in expected directions. These unexpected findings may be due to our limited sample size or heterogeneity in graft sources or treatment regimens. Our study identifies a potential benefit of donor of KIR-B genotypes and absence of L-L mismatch in the GVH direction for pediatric JMML patients. These observations require further investigation for confirmation and understanding of mechanism.
Verneris:Novartis: Membership on an entity's Board of Directors or advisory committees; Fate Therapeutics: Consultancy, Current equity holder in publicly-traded company; Bmogen: Consultancy, Current equity holder in publicly-traded company; Uptodate: Consultancy. Lee:Kiadis Pharma Netherlands B.V: Consultancy, Current equity holder in publicly-traded company, Membership on an entity's Board of Directors or advisory committees, Patents & Royalties.
Author notes
Asterisk with author names denotes non-ASH members.