Proteinuric glomerular diseases are a leading cause of chronic kidney disease (CKD). Both pre-CKD glomerular disease and established CKD are major risk factors for thrombosis. Glomerular capillary podocyte injury is a key determinant of CKD progression and results in massive proteinuria accompanied by an acquired hypercoagulopathy that drives thrombotic risk. Unfortunately, the routine use of anticoagulant prophylaxis during glomerular proteinuria (GP) remains controversial due to both a lack of agreement regarding indications and no randomized controlled trial data demonstrating both safety and efficacy. We have recently used rat glomerular disease models to reveal that: (1) Proteinuria is directly correlated with hypercoagulopathy and in vivo thrombosis and (2) Thrombin, the key effector enzyme of the coagulation system, directly injures podocytes during proteinuria. What is not yet known is the ability of direct oral anticoagulant (DOAC) therapy to improve these important CKD and thrombosis outcomes. Thus, the aim of the present study is to determine if DOACs simultaneously reduce podocytopathy and enable effective thromboprophylaxis during GP. We hypothesized that DOACs would simultaneously preserve podocyte function and reduce hypercoagulopathy, in a podocyte-specific rodent model of glomerular disease.
We utilized the podocin promotor-human diphtheria toxin receptor (pDTR) transgenic rat model to induce highly specific podocyte injury following a single I.P. injection of 50 ng/kg diphtheria toxin (DT). DT-induced proteinuria was subsequently treated daily by oral gavage with 1) Dabigatran (20 mg/kg; Dabi), 2) Rivaroxaban (3 mg/kg; Riva), or 3) Sham (saline) and compared to healthy controls (n=3-6/group). Morning spot urine and citrated plasma samples were collected from each group at day 10 post-DT. Endogenous Thrombin Potential (ETP) was measured by Technothrombin TGA assay, without and with DOAC-Stop reagent. Glomeruli were isolated from the kidney, dissociated into single-cell suspensions and analyzed by flow cytometry following immunofluorescent antibody and TUNEL staining.
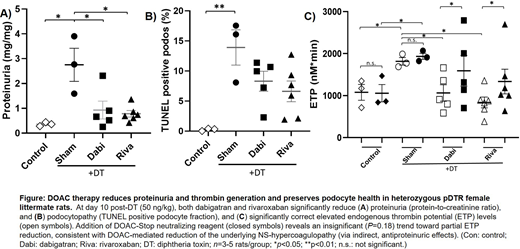
Both Dabi and Riva significantly reduced proteinuria (Fig A) and podocytopathy (TUNEL positive podocyte fraction; Fig B), while concomitantly correcting elevated ETP levels (Fig C open symbols). Addition of DOAC-Stop (Fig C closed symbols) revealed an insignificant (P=0.18) trend toward partial ETP reduction, consistent with DOAC-mediated reduction of the underlying GP-mediated hypercoagulopathy (via indirect, antiproteinuric effects).
In conclusion, dabigatran and rivaroxaban reduce proteinuria and enhance podocyte health in concert with alleviation of the acquired hypercoagulopathy in a podocyte-specific rodent model of glomerular disease. Overall these data suggest DOAC treatment as a novel approach to simultaneously reduce both podocytopathy and thrombotic co-morbidities during glomerular disease. Additional experiments using this model to determine DOAC efficacy on in vivo thrombosis are in progress. Results from these preclinical studies should inform subsequent randomized controlled DOAC trials that may transform care for patients with glomerular disease by mitigating their risk of both CKD progression and thrombosis.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.