Introduction
Despite their high symptomatic burden, frequent quality of life impairment, and possible incurable evolution, patients (pts) with hematological malignancies are hardly ever referred to palliative care (PC) settings. The main reasons explaining the limited resort to PC specialists by hematologists include frequent transfusion need, common infectious complications, possible unpredictable disease course and the growing availability of new and potentially active therapeutic opportunities. Additional factors may include inadequate awareness of the PC landscape, the lack of PC specialist within the hematologic care team and their scarce attitude to address the end-of-life issues with pts and families. Lastly, an intensive psychological bond between pts and their hematologists might contribute to the patient's natural preference of the hospital also for the care of terminal disease. Nonetheless, growing reported experiences confirm an overall worse end-of-life managing outside of the PC specialized settings.
Methods
Starting from 01/2014, in our Institution we started a collaboration with a specialized PC team including both hospice and home settings organization for onco-hematological pts. Aiming to investigate the feasibility of the integration of simultaneous home PC with active and supportive therapies, including transfusion support, for the treatment of pts affected by advanced phase hematological malignancies, we retrospectively collected disease and clinical information from clinical charts of pts who were referred to PC. The database included most relevant information with regard to PC intervention, including evaluation of end-of-life managing. Data were analyzed by descriptive statistics.
Results
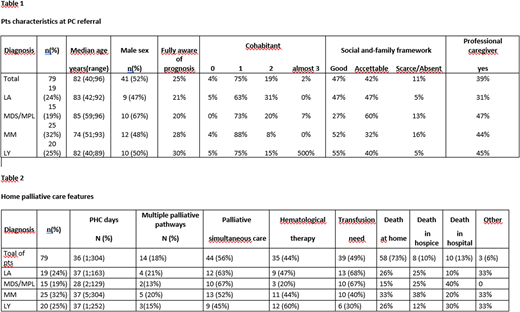
From 01/2014 to 02/2020, 79 pts (52% males) with an onco-hematological disease were referred to home PC. Since 14 pts (18%) required multiple phases of PC assistance during their disease history (12 pts were referred twice and 2 pts three times, respectively), a total of 95 palliative care pathways were identified. Pts characteristics at PC referral are listed in table 1. Median age at the time of referral to PC was 82 years (range 40-96). Onco-hematological disease was acute leukemia (AL) in 25%, multiple myeloma (MM) in 32%, lymphoma in 25% and myelodysplastic syndrome (MDS) or myeloproliferative neoplasms (MPN) in 19% of patients. 95% of pts were informed of their diagnosis, but only 25% of pts were fully aware of the prognosis. With 75% of pts permanently living with a relative and 4% living alone, family framework was considered fully appropriate in 47% of pts, acceptable in 42% and scarce in 11%; altogether, a professional caregiver was present in 39% of pts.
At the home PC referral, only 24% of pts was self-sufficient in daily activities, even though 78% was totally conscious. Overall, 36% of the pts complained at least 3 relevant symptoms among pain, hallucination, confusion, agitation, sleep disorders, dyspnea, nausea, asthenia, anxiety and psychological distress.
Median duration of the home PC was 36 days, widely ranging from 1 up to 304 days. Simultaneous PC occurred in 44 pts (56%), while 35 pts (44%) continued a primarily oral hematological therapy. 39 pts (49%) received blood components transfusions in the hospital during the home PC assistance, in accord with the PC specialist. Death eventually occurred at home in 58 patients (73%), in hospice in 8 patients (10%), and in hospital in 10 patients (13%) [Table 2].
Conclusions
The population referred to our home PC organization included pts with various hematological malignancies. During home PC assistance, 56% of the pts continued to attend our onco-hematology department for monitoring visit during an ongoing oral hematological therapy (44%) and/or for blood transfusion support (49%).
With the vast majority of pts eventually deceasing at home or in hospice, the integration of home PC both with active hematology treatment and transfusion support appears to be feasible, meaningfully improving end of life management of patients with advanced hematological malignancies.
The experience of multiple home PC pathways during the disease course in a proportion of patients offers an interesting perspective for a possible planning of temporarily palliative support in onco-hematological pts, who sometimes could still strikingly benefit of active treatments, even in very advanced phase of their disease.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.