Background:
Bronchiolitis obliterans syndrome (BOS), also known as respiratory chronic Graft versus Host Disease (cGvHD) is an obstructive airway disease of the lungs mainly associated with alloHSCT or lung transplantation. BOS is characterized by T-cell mediated inflammation and fibrosis of bronchiolar walls that reduces the diameter of the bronchioles resulting in progressive and irreversible airflow obstruction.
BOS is a well described complication following lung transplant with a 5-year prevalence rate of 50%. It can also be a complication following alloHSCT with similar histopathology and clinical symptoms. Currently, there are no approved treatments for BOS. The aim of this study is to describe the prevalence of BOS following alloHSCT.
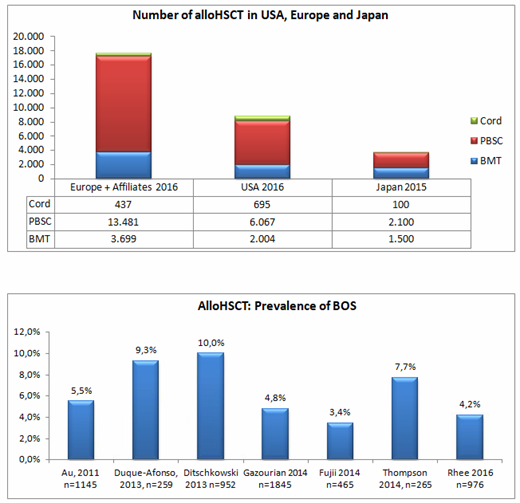
A review and analysis of the following data sources was performed: AlloHSCT activity reports from The European Society for Blood and Marrow Transplant 2016 the Center for International Blood and Marrow Transplant Research 2016, and the Japanese Data Center Hematopoeitic Stem Cell Transplantation 2015 in order to identify the number of procedures performed. Further a PubMED literature search was also conducted and identified publications with > 100 patients using the key terms "bronchiolitis obliterans and haematopoietic stem cell", and "bronchiolitis obliterans after stem cell transplant" from 2011 to 2017. Case reports and redundant publications were excluded from the analysis.
Results
Approximately 30,000 alloHSCTs were performed each year in the USA (8766 in 2016), Europe (17,617 in 2016) and Japan (3700 in 2015). Based on seven eligible studies published between 2011 and 2016, the reported prevalence of BOS in patients who underwent alloHSCT ranged from 3.4% to 10%. Median time to diagnosis of BOS following alloHSCT was 273 to 547 days post-transplant. Those with routine Forced Expiratory Volume at 1 second (FEV1) monitoring had a higher likelihood of being diagnosed with BOS and a shorter time to diagnosis.
Conclusion
Based on estimated prevalence, up to 3000 patients following alloHSCT per year could be diagnosed with BOS. Routine monitoring may positively impact early and shorten time to diagnosis and allow treating such a population.
Hofstetter:Breath Therapeutics GmbH: Consultancy. Henig:Breath Therapeutics Inc.: Employment. Kappeler:Breath Therapeutics GmbH: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.