Background:
Renal medullary carcinoma (RMC) is a rare, aggressive form of renal cell carcinoma almost exclusively (>90%) diagnosed in individuals with sickle cell trait (SCT), and 2/3 of those affected are male. Based on population-surveillance data, only 246 patients were diagnosed with RMC between 2005-2014 (Carden etal. J Sickle Cell Disease and Hemoglobinopathies, 2018) and many patients have metastatic disease at diagnosis (Msaeoul et al., Clin Genitourin Cancer, 2019). Median overall survival (OS) in patients with metastatic RMC (mRMC) at diagnosis is less than 12 months and predictors of survival are largely unknown, although case reports suggest novel chemotherapeutic strategies are important (Carden et al., Ped Blood Cancer, 2017&2018). The role SCT plays in RMC pathobiology, however, is largely unknown, as many patients do not have a complete hemoglobin subtype profile completed at diagnosis. Studies evaluating sickle hemoglobin concentrations (%HbS) in relation to survival for patients with RMC are needed, as SCT is associated with renal dysfunction and researchers have hypothesized that HbS polymerization within red cells traversing the kidney disrupts blood perfusion, which leads to kidney injury and an increased possibility for cancer formation (Msaeoul et al, Clin Cancer Res, 2018). Patients with %HbS≤36%, such as patients with SCT and concomitant alpha-globin gene deletion(s) might be protected against HbS polymerization and renal concentrating defects (Gupta etal., J Clin Invest, 1991). We hypothesize that lower %HbS is associated with higher survival. In this preliminary multi-institutional study, we retrospectively reviewed available charts from patients diagnosed with mRMC and SCT to evaluate for an association between %HbS and OS.
Methods:
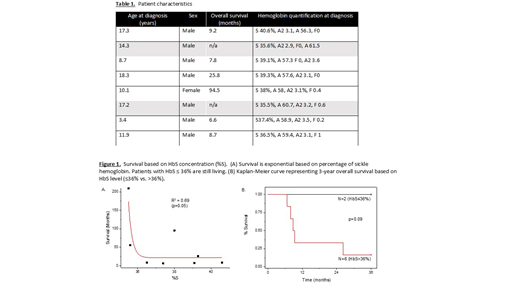
We found nine patients (3 adults, 6 children) who were diagnosed with mRMC and SCT at our various institutions between 2002-2017 who had survival data. Eight patients had %HbS levels by hemoglobin quantification at diagnosis. In a post-hoc analysis, patients were separated into two groups (%HbS>36% and %HbS≤36%), levels similar to that found in patients with alpha-globin gene deletions described by Gupta et al. Fit-curves were determined for OS vs. %HbS. Three-year OS was determined using Kaplan-Meier analysis and the log-rank method. P<0.05 was considered statistically significant.
Results:
Clinical characteristics of patients are shown in Table 1. Average age (standard deviation) at diagnosis was 15.2 years (4.9) and most patients were male (87.5%). Six patients had %HbS >36% and 2 patients had %HbS ≤36%. Median OS was 17.8 months. Using fit-function testing, analysis of survival vs. %HbS yielded an exponential relationship (R2=0.69), suggesting higher survival when %HbS≤36% (p=0.05). OS of the two patients with %HbS≤36% was greater than those with %HbS>36%, though results were not statistically significant (p = 0.09).
Conclusion:
While there are limitations to this small, retrospective analysis, these data suggest that lower intracellular red cell %HbS concentrations could be protective in patients with mRMC and SCT. Chemotherapy and other treatment regimens may also play a role in survival and need to be studied. Further investigation is needed to determine the role SCT plays in RMC pathobiology and to determine if %HbS concentrations, as well as alpha-thalassemia deletion(s), may be protective in patients with RMC.
Carden:GBT: Honoraria; NIH: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.