Introduction: There have been great strides in lymphoma treatment options and patients' health outcomes but one area of lymphoma care that seems to have been left behind is ensuring patient-centred medical practice. The complexity of the lymphoma experience and the myriads of side effects from treatments makes patient-centricity a cornerstone for the care of lymphoma patients. Communication with the clinicians is a significant component of this. This study describes the experiences and unmet needs in patient-doctor communication of patients (FL and DLBCL) using the Lymphoma Coalition (LC) 2018 Global Patient Survey (GPS) on Lymphomas and CLL.
Methods: Globally, 6631 participants took part (70+ countries) in the 2018 LC GPS. There were 937 FL and 1478 DLBCL respondents. Demographics of both groups of patients were examined and questions relating to patient-doctor experiences and perceptions were examined. Descriptive analysis was performed. Differences in proportions was tested through chi-square tests (p=0.05). Statistical analyses was performed with IBM SPSS v21.
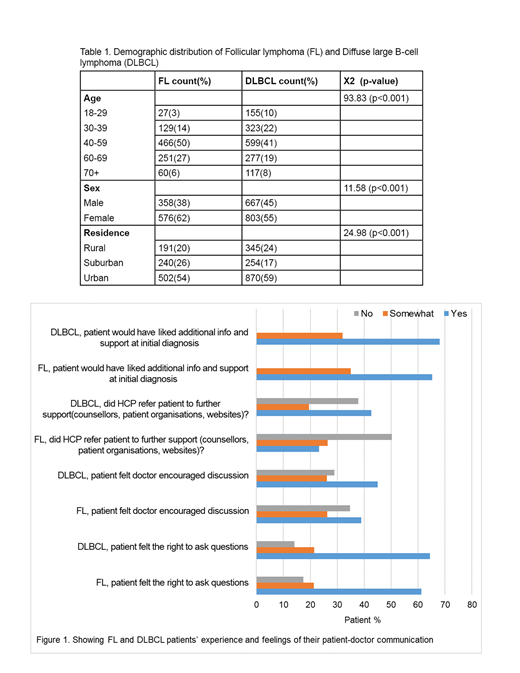
Results: FL and DLBCL respondents differed in the distribution of age, sex, and residence (all p values <0.05) (table 1). A third of DLBCL patients (32%) were <40 years in age compared to 17% of FL patients. On the other hand, there were more older patients (>60 years) in the FL group (33%) compared to the DLBCL group (27%). Two -thirds of FL respondents were females (62%) compared to 55% of DLBCL patients. One-fifth (20%) of FL patients and 24% of DLBCL patients resided in rural areas.
Two-thirds of both groups (FL-65%, DLBCL-68%) would have liked more information and support at their initial diagnosis. Despite this need, less than half of the patients felt their doctors encouraged discussion (FL-39%, DLBCL-45%) and only 23% of FL and 43% of DLBCL patients were referred to further avenues of support (figure 1).
Most patients (FL-70%, DLBCL-77%) reported communicating their medical/physical issues to their doctors compared to the low level of communication of emotional issues in both groups (FL-41%, DLBCL-38%). For those who communicated issues, less than half of them felt helped by their doctors for physical issues (FL-40%, DLBCL-47%) and less still for emotional issues (FL-31%, DLBCL-42%).
Patients' unmet need for help with fatigue, fear of cancer relapse (FOR) and side effects were also examined. Fewer patients felt the doctor helped with issues of fatigue (FL-33%, DLBCL-43%) and FOR (FL-33%, DLBCL-40%) compared to helping out with treatment side effects (62%-FL, 69%-DLBCL).
Patients' unmet need for help with fatigue, fear of cancer relapse (FOR) and side effects were also examined. Fewer patients felt the doctor helped with issues of fatigue (FL-33%, DLBCL-43%) and FOR (FL-33%, DLBCL-40%) compared to helping out with treatment side effects (62%-FL, 69%-DLBCL).
Conclusion: The results show that FL and DLBCL patients would like more information and support than currently provided by their doctors. Doctors are more likely to address physical aspects of care. A large gap exists regarding communication surrounding the emotional/psychosocial issues that lymphoma patients' experience. LC advocates for stronger patient-centered care that addresses these gaps in communication.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.