Background
Acute myeloid leukemia (AML) is a common hematologic neoplasm in the elderly. The high mortality in elderly AML patients is reported to be associated with old age, poor performance status, and several disease characteristics. Several risk stratification models have been reported. Our aims were to explore risk factors for early mortality in older AML patients and compare the discrimination ability of existing prognostic models.
Methods
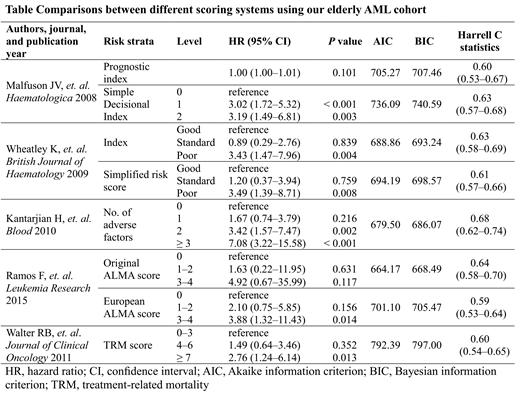
We enrolled newly diagnosed AML patients age 60 and above at Taipei Veterans General Hospital, a national medical center in Taiwan, between July 1, 2008 and May 31, 2017. Our primary endpoint was early mortality, defined as death within two months after initial AML diagnosis. Performance of several existing scoring systems were compared by using the Akaike information criteria (AIC) and Bayesian information criterion (BIC) calculations. Model discrimination ability was also estimated by Harrell's C statistics.
Results
A total of 478 AML patients were diagnosed during the eight-year follow-up period. After excluding young patients (age < 60) and those without a histopathologic diagnosis, the final cohort included 277 patients. The median age was 74 (range 60-96), and 171 (61.7%) of them were male. One hundred sixteen patients (41.9%) had Eastern Cooperative Oncology Group performance (ECOG) ≥ 2 and 33.9% patients had poor/adverse cytogenetics or molecular abnormalities. The two-month mortality rate was 29.9% (95% confidence interval [CI] 24.8%-35.9%). Age ≥ 80 (adjusted HR 1.95, 95% CI 1.12-3.42), having an antecedent hematologic disorder (adjusted HR 1.86, 95% CI 1.01-3.43), ECOG ≥ 2 (adjusted HR 2.06, 95% CI 1.20-3.54), complex karyotype (adjusted HR 3.13, 95% CI 1.76-5.55), BM blasts ≥ 70% (adjusted HR 1.79, 95% CI 1.02-3.13), WBC ≥ 100 ×109/L (adjusted HR 3.27, 95% CI 1.58-6.75), and creatinine > 1.3 mg/dL (adjusted HR 2.04, 95% CI 1.23-3.39) were identified as independent predictors for early mortality in the multivariate analysis. Furthermore, we systematically reviewed existing prognostic models for elderly AML. We found five scoring models that don't require additional specific examinations beyond clinical practice and later applied them to our elderly AML cohort. The performance of the five models is shown in Table. Kantarjian's prognostic model (Kantarjian H, et. al. Blood 2010) had the highest Harrell's C statistic and the ALMA score (Ramos F, et. al.Leukemia Research 2015) had the lowest AIC and BIC compared with the other prognostic models.
Conclusion
We identified seven risk factors for early mortality and compared the performance of five prognostic models for elderly AML patients. The finding may help clinicians to stratify patients and initiate appropriate management.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.