Background:
Pulmonary embolism (PE) is an important cause of morbidity and mortality and represents one of the most common causes of cardiovascular death after myocardial infarction and stroke. Despite advances in the management of PE over the past decade, it is unknown whether mortality from PE has significantly changed. Therefore, our objective was to describe trends in death rates due to PE in the United States from 1999-2017, as well as to examine mortality trends by age, sex and race.
Methods:
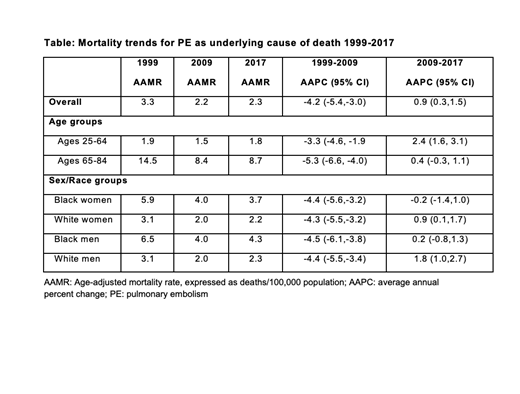
We used death certificate data from the Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research from January 1, 1999, to December 31, 2017, to calculate age-adjusted mortality rates (AAMR) per 100,000 population for PE (ICD-10 code I26) listed as underlying cause of death. AAMRs were examined overall, as well as by age (25-64 years versus 65-85 years) and sex/race groups. The Joinpoint Regression Program (National Cancer Institute) was used to identify up to one inflection point in AAMR trends. Statistical trends and average annual percent change (AAPC) were examined over the study period.
Results:
Between 1999 and 2017, there were 152,463 deaths attributable to PE as underlying cause of death. AAMR due to PE experienced an inflection point in 2009. AAMR was 3.3, 2.2, and 2.3 per 100,000 in 1999, 2009, and 2017, respectively. Trends in PE mortality rates reversed after the inflection point, with an AAPC before 2009 of -4.2% (-5.4, -3.0, p<0.001), indicating reduction in AAMR of 4.2% per year between 1999 to 2009, versus AAPC of +0.9% (0.3, 1.5, p<0.001) after 2009. When examined by age group (25-64, 65-84 years), the AAMR decreased between 1999 to 2009 for both age groups. Between 2009-2017, the AAMR for older adults (65-84 years) plateaued (AAPC 0.4% (-0.3, 1.1), while the AAMR for younger adults (25-64 years) increased (AAPC 2.4% (1.6, 3.1). Examination by sex/race groups demonstrated similar patterns of change with decrease in AAMR between 1999-2009 and plateau or increase in AAMR after 2009 (Table). Throughout the study period, black men and women had approximately a 2-fold higher AAMR compared to white men and white women.
Conclusion:
We provide contemporary nationwide estimates of trends in PE mortality over the last 18 years. In the past decade, death rates due to PE have become stagnant, reversing the trend from the prior decade where mortality rates were decreasing. Premature death attributable to PE showed a rising trend, which may be driving the overall reversal during the study period. Furthermore, racial disparities exist in mortality due to PE, with black men and women consistently having higher AAMR compared to white men and women. Identification of the underlying cause of the plateau in mortality rates and persistently observed disparities are needed in order to improve outcomes related to PE equitably and prevent reversal toward increasing mortality trend due to PE.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.