Introduction: Survival of Multiple Myeloma (MM) patients has improved in recent decades due to the advent of novel agents and broader utilization of stem cell transplant. Fatal outcomes occur mostly after multiple lines of therapy due to increasingly resistant disease. Indeed, early mortality after diagnosis is unusual in front line treatment MM trials, where patients are often selected on the basis of good performance status and absence of organ dysfunction. The real world incidence of early deaths is largely unknown. Hereby, we analyze the factors impacting early mortality in the National Cancer Database (NCDB) which covers more than 70% of MM patients in United States.
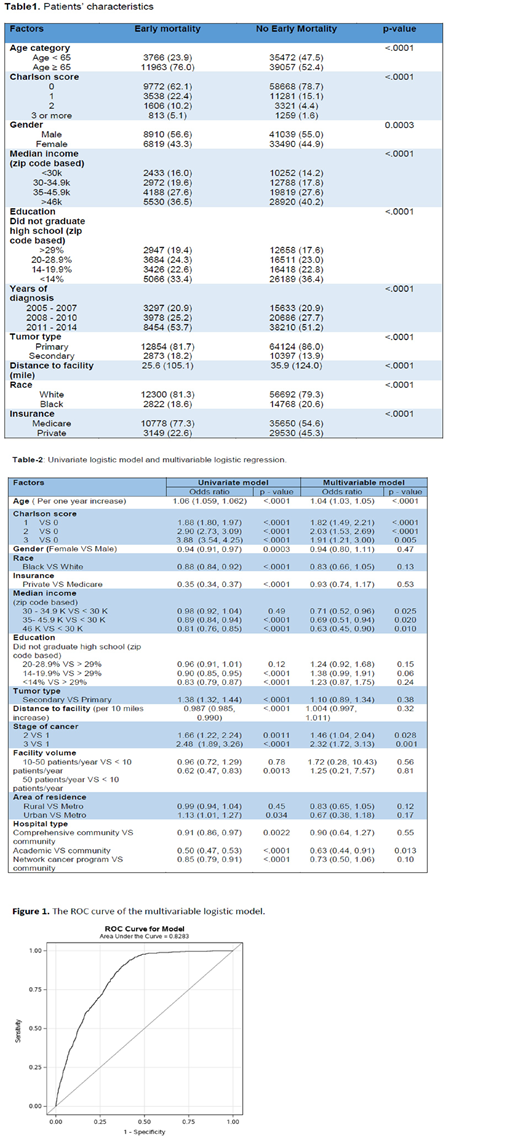
Methods: Patients with MM diagnosed from 2005-2014 were identified in the NCDB. Early mortality (EM) was defined as death within six months of MM diagnosis. The effect of demographic and clinical factors, insurance type, distance to treatment facility, medical facility and facility volume on the probability of EM was estimated by univariate logistic model. The effect of these factors on the probability of EM was further estimated by multivariable logistic regression. The overall performance of multivariable logistic regression was evaluated using the receiver operating characteristic curve (ROC) analysis. The difference of continuous measurements between groups was examined using t-test. The association between categorical variables was examined using Chi-square test. All tests are two-sided and p-value ≤ 0.05 were considered statistically significant.
Results: 90,258 patients with ICD-O 9732 were included. 49949 (55%) were male. EM was reported in 15729 (17%) within the first 6 months after MM diagnosis. Median age at diagnosis was 67 years (19-90). 15729 patients (17%) died in the first 6 months after diagnosis. There was no significant change in the percentage of EM over the years from 2005-2014. 11963 (76%) of patients with EM were older than 65 years while 3766 (23%) patients were less than 65 years. 12300 (78.1%) of the patients with EM were white and 2822 (17.9%) were African American.
In a multivariable analysis, variables that confer the worst prognosis were increasing age, higher charlson co-morbidity score, lower annual median income of less than 30,000, and being treated in a community hospital. Controlling the effects of other factors (charlson co-morbidity score, hospital type and transplant), the odds ratio of EM was 1.04 per year increase of age (p<0.0001), 0.52 with treatment in academic center compared to community hospital (p<0.0001).
Conclusion: Taken together our data suggest almost 1 out of 6 MM patients died at the first 6 months after diagnosis. Therefore, EM remains high in MM and a major barrier for continued improvement in survival outcomes. In addition to well-known MM-specific determinants of survival, socioeconomic factors were significantly associated with early mortality.
Malek:Adaptive: Consultancy; Medpacto: Research Funding; Janssen: Speakers Bureau; Sanofi: Consultancy; Celgene: Consultancy; Takeda: Consultancy; Amgen: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.