Introduction: The majority of patients with classical Hodgkin lymphoma (cHL) will be cured with anthracycline-containing chemotherapy regimens. However, 10-20% of patients with early-stage disease and 30-40% of patients with advanced-stage cHL will relapse. The standard treatment for patients with relapsed cHL is salvage chemoimmunotherapy followed by high-dose chemotherapy (HDT) and autologous hematopoietic cell transplantation (auto-HCT) in chemotherapy-sensitive patients. Patients with primary treatment failure (PTF), i.e. patients who have progressive disease while on therapy or who fail to achieve complete remission (CR) at the end of initial therapy, or experience early relapse after CR1 are expected to have a worse prognosis than patients with late relapse. Since 2011 newer treatments, namely Brentuximab vedotin and PD1/PDL1 blockers have been introduced for the treatment of relapsed and refractory cHL. It is unknown whether changes in disease monitoring and management, including the availability of new agents, impacted survival of patients with cHL and PTF.
Methods: Fifteen US academic medical centers contributed cases to the ECLIPSE study (Evaluation of Classical Hodgkin Lymphoma patients wIth Primary treatment failure and analySis of outcomEs). ECLIPSE retrospectively captured patient, disease and treatment characteristics and treatment response as assessed by treating physicians. Eligible patients were ≥ 15 years diagnosed with cHL on or after 2005, who received treatment with curative intent with anthracycline-containing chemotherapy regimens, and developed one of the 3 patterns of PTF: detection of progressive disease during or within 6 weeks of completion of chemotherapy (PP cohort, primary progression), partial response (PR) or stable disease (SD) by functional imaging at completion of chemotherapy (PR/SD cohort), or disease progression detected within 12 months of completion of chemotherapy after prior documentation of CR (ER cohort, early relapse). Patients were divided into two "eras" based on year of diagnosis, 2005-2010 (era1) and 2011-2018 (era2), with the latter expected to reflect changes in salvage therapy for cHL.
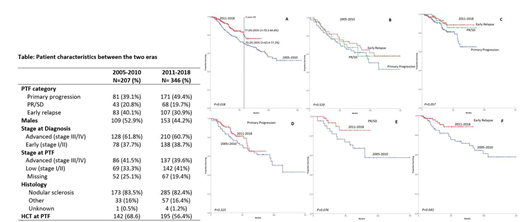
Results: Patient characteristics for the 553 cases are summarized in Table. Median follow up of survivors was 58.7 and 31.2 months for patients diagnosed in era1 and era2, respectively. ABVD was the upfront treatment for 97.6% of cases. Nearly all patients (98.5%) received salvage therapy after PTF and 60.9% underwent auto-HCT. Patients who relapsed or progressed post auto-HCT received a median of 1 (range 0 to 3) salvage regimens. Five-year overall survival (OS) from time of PTF was 70.3% (95% CI=63.4-77.2%) for patients diagnosed in era1, and 77.6% (95% CI=70.3-84.8%, p = 0.018) for patients diagnosed in era2 (Figure A). While there was no difference in OS among the PP, PR/SD and ER cohorts in the era1 (Figure B), the PR/SD and ER cohorts had better OS than PP cohort in era2 (Figure C). On comparing the OS for each of the 3 cohorts between era1 and era2, there was an improvement in OS in the PR/SD (Figure E) and ER cohorts (Figure F) but no improvement among the PP cohort (D). Multivariable analysis of patients in era 2 identified only age (HR 1.05, 95% CI=1.03-1.07, P<0.001) and PP pattern of PTF (HR 2.45, 95% CI=1.11-5.40, P=0.03) as predictors of worse survival.
Conclusions: Though there has been an improvement in survival among cHL cases with PTF treated in the most recent years, the outcome of patients with PP did not change significantly across eras. Patients with PP disease should be prioritized for clinical trials incorporating newer agents and innovative cellular therapy to current available effective treatments.
Epperla:Pharmacyclics: Honoraria; Verastem Oncology: Speakers Bureau. Costa:Abbvie: Consultancy; Karyopharm: Consultancy; Fujimoto Pharmaceutical Corporation Japan: Other: Advisor; Sanofi: Consultancy, Honoraria, Speakers Bureau; GSK: Consultancy, Honoraria, Research Funding; Amgen: Consultancy, Honoraria, Research Funding, Speakers Bureau; Janssen: Research Funding, Speakers Bureau; Celgene: Consultancy, Honoraria, Research Funding. Cashen:Novartis: Other: Speaker's Bureau; Seattle Genetics: Other: Speaker's Bureau; Celgene: Other: Speaker's Bureau. Hamadani:Otsuka: Research Funding; Takeda: Research Funding; Pharmacyclics: Consultancy; ADC Therapeutics: Consultancy, Research Funding; Merck: Research Funding; Sanofi Genzyme: Research Funding, Speakers Bureau; Celgene: Consultancy; Janssen: Consultancy; Medimmune: Consultancy, Research Funding. Barta:Mundipharma: Honoraria; Celgene: Research Funding; Takeda: Research Funding; Janssen: Membership on an entity's Board of Directors or advisory committees; Seattle Genetics: Honoraria, Research Funding; Bayer: Consultancy, Research Funding; Mundipharma: Honoraria; Merck: Research Funding; Celgene: Research Funding; Janssen: Membership on an entity's Board of Directors or advisory committees. Reddy:Celgene: Consultancy; BMS: Consultancy, Research Funding; Genentech: Research Funding; Abbvie: Consultancy; KITE Pharma: Consultancy. Karmali:Gilead/Kite; Juno/Celgene: Consultancy, Speakers Bureau; Takeda, BMS: Other: Research Funding to Institution; Astrazeneca: Speakers Bureau. Bello:Celgene: Speakers Bureau. Chavez:Novartis: Membership on an entity's Board of Directors or advisory committees; Kite: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Bayer: Membership on an entity's Board of Directors or advisory committees; Karyopharm: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees; Genentech: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Svoboda:AstraZeneca: Consultancy; Celgene: Research Funding; Incyte: Research Funding; Pharmacyclics: Consultancy, Research Funding; Kyowa: Consultancy; Merck: Research Funding; BMS: Consultancy, Research Funding; Seattle Genetics: Consultancy, Research Funding. Glenn:BMS: Research Funding; Merck: Research Funding; Genentech: Research Funding. Cohen:Lymphoma Research Foundation: Research Funding; Seattle Genetics, Inc.: Consultancy, Research Funding; ASH: Research Funding; Takeda Pharmaceuticals North America, Inc.: Research Funding; Gilead/Kite: Consultancy; Bristol-Meyers Squibb Company: Research Funding; Genentech, Inc.: Consultancy, Research Funding; Janssen Pharmaceuticals: Consultancy; LAM Therapeutics: Research Funding; UNUM: Research Funding; Hutchison: Research Funding; Astra Zeneca: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.