TO THE EDITOR:
Benign hematology consultations constitute a sizable proportion of the evaluation requests in traditional hematology/oncology practices. There is a need for physicians with adequate training, experience, interest, and expertise in assessing and treating patients with these disorders.1-3 Some hematologic issues are complex and require in-person histories and examinations, whereas others can be handled with advice electronically after a thorough chart review.4 To improve the quality of the care provided to these patients, a virtual benign hematology consultative service was created.
This program was developed within a multispecialty group operating under a capitated reimbursement model, with a commonly accessible electronic medical record, servicing 15 medical service area centers, each with their own hematology/oncology department. After receiving buy-in from the department of adult and family medicine, a pilot project was initiated in October 2017 between 2 participating medical centers. It was expanded to include a total of 5 medical centers by March 2018. All nonurgent benign hematology consultation requests were submitted electronically through an “e-consult” portal. Evidence-based workups for discrete common hematologic conditions were developed with consensus among all 15 hematology departments and provided on the e-consultation landing pages. These were the primary workups that would evaluate for common causes; secondary and tertiary testing was left to the discretion of the triaging hematologist and not published on the triage algorithm. All urgent questions and in-patient consults were called in directly to an on-call physician. The services included an electronic consultation, where advice was provided to the primary care physician or an in-person visit with the patient directly. The advice given to the referring provider was asynchronous, involved review of the chart with documentation of recommendations in the medical record, and did not use direct communication between the patient and specialist. 5,6 An in-person appointment was synchronous, face-to-face with the patient, and follow-up was with the specialist.
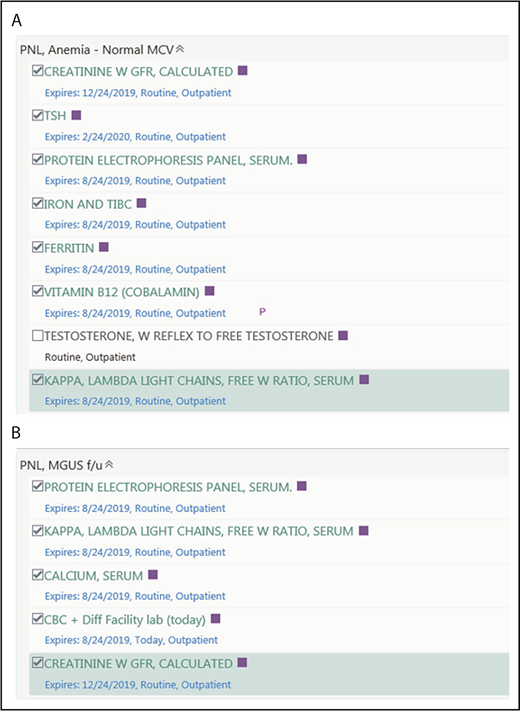
To foster development of expertise and to use fewer physicians in this work, medical centers were combined into groups of 2 to 3. One hematology physician from each medical center would rotate weekly in triaging consults for the centers within their respective pairing. Given our capitated model of payment, no change in reimbursement structures were needed, and work was incentivized by shifting in-person consultation duties for the department to other partners during this period. Prepopulated templates that could be called up electronically were developed to answer frequently asked questions, thereby automating repetitive tasks and generating consistency in the responses. Ordering panels for the workup of common hematologic issues were designed to help make the evaluation of these patients more streamlined and evidence based (Figure 1A-B). This allowed for the referring providers to choose more wisely the tests they ordered. Blood smears were reviewed by a local hematopathologist with findings documented in the electronic chart; the slide was subsequently archived and available for review by the evaluating hematologist.
Ordering panels (PNL). (A) Ordering panel for anemia with a normal mean corpuscular volume (MCV). The panel allows for tests to be added or removed as appropriate. It can be called up in the electronic chart by typing in “anemia normal MCV” in the orders section. (B) A panel for follow-up (f/u) for patients diagnosed with monoclonal gammopathy of uncertain significance (MGUS). These orders can be entered as standing orders to be drawn every 1 to 3 years as requested by the ordering physician.
Ordering panels (PNL). (A) Ordering panel for anemia with a normal mean corpuscular volume (MCV). The panel allows for tests to be added or removed as appropriate. It can be called up in the electronic chart by typing in “anemia normal MCV” in the orders section. (B) A panel for follow-up (f/u) for patients diagnosed with monoclonal gammopathy of uncertain significance (MGUS). These orders can be entered as standing orders to be drawn every 1 to 3 years as requested by the ordering physician.
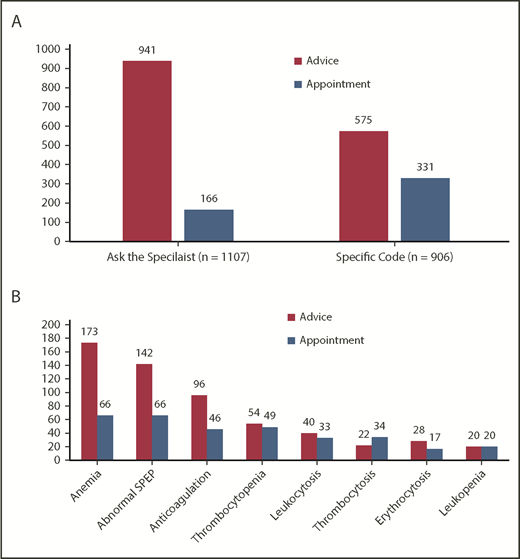
The pilot project was initiated in October 2017, and data from this date through April 2018 are reported. During this 7-month period, there were 2013 consults submitted electronically for review. Of this, 1107 came under the nonspecific “Ask the Specialist” code, and 906 came under a specific diagnosis code. Regarding the consults with a designated diagnosis code, anemia 239 (11.9%), abnormal serum protein electrophoresis 208 (10.3%), anticoagulation 142 (7.1%), thrombocytopenia 103 (5.1%), leukocytosis 73 (3.6%), thrombocytosis 56 (2.8%), erythrocytosis 45 (2.2%), and leukopenia 40 (2.0%) were the most common inquiries. The requests that came under the “Ask the Specialist” code included questions regarding iron deficiency, easy bruising, macrocytosis without anemia, hypercoagulable testing question, elevated ferritin levels, multiple complete blood count abnormalities, elevated prothrombin time/partial thromboplastin time, hemoglobinopathies, and a personal bleeding history to name a few. Of these 1107 “Ask the Specialist” consults, 941 (85.0%) were handled with advice given electronically, whereas 116 (15%) were triaged to an in-person appointment. When evaluating the specific diagnosis codes, out of 906 total consults, 575 (63.4%) were handled with advice given electronically. By percentage of consults received, the most commonly triaged diagnoses for in-person appointments were thrombocytosis (60.8%), leukopenia (50.0%), and thrombocytopenia (47.6%), typically for an in-depth examination or for a diagnostic bone marrow biopsy (Figure 2A-B). Of the consultation requests, 90.3% were addressed within 24 hours. This included advice documented in the chart to the referring provider or triaging the consult to an appointment. All appointments were offered within 7 days unless the patient requested a later date. We also evaluated the number of consults that were addressed on each day of the week between paired centers. An average of 32.7, 25.8, 19.6, 24.4, and 18.2 consults were triaged Monday through Friday, respectively, across all medical centers.
Triage outcomes. (A) Triage outcomes for the entire cohort based on referral as a generic “Ask the Specialist” code or a specific code. The red bars represent the number of consults closed with advice given to the referring provider, whereas the blue bars represent the number of consults triaged to an in-person appointment. (B) Triage outcomes for the specific code cohort by diagnosis. SPEP, serum protein electrophoresis.
Triage outcomes. (A) Triage outcomes for the entire cohort based on referral as a generic “Ask the Specialist” code or a specific code. The red bars represent the number of consults closed with advice given to the referring provider, whereas the blue bars represent the number of consults triaged to an in-person appointment. (B) Triage outcomes for the specific code cohort by diagnosis. SPEP, serum protein electrophoresis.
The time necessary to complete an electronic consultation was calculated based on data from 7 hematologists. With a sample size of 197 consults, an average of 14.47 minutes was required to complete each electronic consultation (95% confidence interval, 14.02 to14.91 minutes). This is identical to what was reported by Cecchini et al in their experience with a similar program at the VA health system.4
All referring physicians were surveyed regarding their perceptions of the program and were asked to scale their responses from 1 to 5. When asked if the workup algorithms were concise, whether the workup was relevant to the patient, and whether the recommendations received were clear/helpful, the weighted average responses were 4.70, 4.61, and 4.50, respectively. All 7 hematology providers who participated in the initial pilot reported their perception of the program changed to a strongly positive view after participating over a 3-month period.7 To improve consistency and expand capacity, a 1-hour weekly case conference was developed for hematologists to present cases for discussion. This created a forum to discuss challenging diagnoses and harmonize differences in opinions, leading to improvements in proficiency and ultimately patient care.
The future of benign hematology as a specialty is being shaped by restructured reimbursement models, changes in the workforce supplying this care, and fellowship programs developing an emphasis on training physicians in malignant hematology and oncology.3 Opportunities to leverage the expertise of fewer physicians with experience in caring for patients with benign hematologic conditions would add significant value to health care systems. This was a pilot program to assess the feasibility of a virtual hematology consultative service, whereby a larger number of patients with hematologic abnormalities can have their cases reviewed by an expert. The initial success of the program shows that it is possible to provide high-value consultations to referring providers in an expeditious manner that enhances quality of care. Patients are also spared a visit to the hematology/oncology clinic to discuss a benign condition and therefore have the added benefit of reduced anxiety, and simultaneous improved access for patients who do need to be seen in person.8 What is unique about this program is that it brought together physicians from the same specialty across multiple medical centers under 1 service platform. A capitated model of reimbursement incentivizes quality and efficiency, allowing this program to fit simply into this paradigm of care. Fee-for-service models can use this program by having providers bill for the time spent on each consult and by negotiating fees with payers or medical group administrators looking for cost-effective options that streamline patient care.
In conclusion, the program is expected to be used by all 15 hematology departments by early 2019. Future studies will involve measuring outcomes of patients who were managed virtually, and the effect of the recommendations on the use of tests. The ongoing goal is to develop, grow, and sustain a core benign hematology program given the critical importance this field has to the care of patients in the community.
Presented in abstract form at the 60th annual meeting of the American Society of Hematology, San Diego, CA, 1-4 December 2018.
Acknowledgments
The authors thank Jahan Tavakoli, Alfredo Lopez, Amy Nelson, Jerome Kim, Natalya Greyz, Aruna Gavini, Shafqat Akhtar, Nicolaj Andersen, Douglas Kaufman, Aram Canin, and Juraj Kavecansky for their participation in the virtual hematology consult service.
Authorship
Contribution: A.P. developed the program, analyzed the data, and wrote the manuscript; D.K. and T.K. developed the program; and N.F., K.R., and K.K. developed the program and collected the data.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Ashok Pai, Kaiser Permanente Oakland Medical Center, 3701 Broadway, 3rd Floor, Oakland, CA 94611; e-mail: ashok.p.pai@kp.org.