Abstract
Introduction: Treatment with Rituximab has improved the outcome for patients with B-cell precursor ALL (B-ALL) and is conventionally restricted to patients with CD20 expression on leukemic blasts above a level of 20%. However, it is not known whether this arbitrary cutoff is biologically meaningful, or if also patients with lower CD20 expression levels profit from Rituximab treatment. In addition, CD20 expression levels might differ between different compartments and can change during early treatment. Therefore, in the current German Multicentric Acute Lymphoblastic Leukemia (GMALL) 08/2013 trial Rituximab is applied to all BCR-ABL1-negative B-ALL patients during induction and early consolidation irrespective of the initial blast CD20 expression. In this study, CD20 expression on blasts at diagnosis and after a 5-day dexamethasone prephase is thoroughly characterized and correlated to MRD response after induction I including one dose of Rituximab to evaluate its impact on response to Rituximab.
Methods: Comparative quantification of CD20 expression levels was performed at diagnosis (blood and bone marrow (BM)) and at the end of the prephase (blood) and correlated to minimal residual disease (MRD) response after early Rituximab treatment. Samples were subjected to the EuroFlow standardized stain, lyse and wash and instrument setting procedures (van Dongen et al., 2012) and stained with a 3-tube, 8-color panel, containing the markers CD45, CD20, CD10, CD66c, CD3, CD19, CD71, CD9, CD13+33, CD34, CD22, CD11a, and CD38. CD20 median fluorescence intensities (CD20-MFI) as well as percentages of CD20+ B-ALL blasts among all blasts (%CD20+) were measured. MRD was quantified at day 22 after induction I using real-time quantitative PCR of clonal immune gene rearrangements. MRD response after induction was defined as MRD decrease to a level below 10-4, MRD persistence as detection of quantifiable MRD ≥10-4.
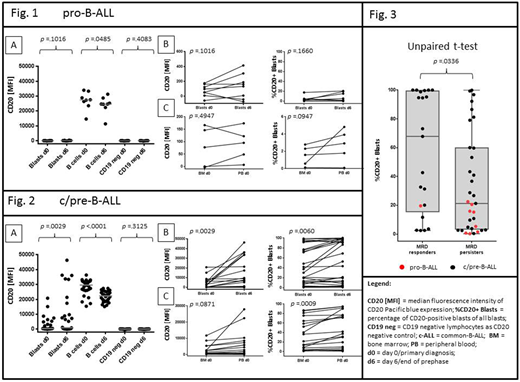
Results: FCM results of a total of 166 samples of 84 B-ALL patients were evaluated. CD20 expression of circulating blasts significantly increased after a 5-day prephase in common/pre-B-ALL (c/pre-B) but not in pro-B-ALL in a cohort of 36 paired peripheral blood samples (Fig. 1 A-B, n=8 pro-B-ALL, paired t-test of CD20-MFI and %CD20: p=.1016 and p=.1660, Fig. 2 A-B, n=28 c/pre-B-ALL, p=.0029 and p=0.0060). Interestingly, the increase of CD20 expression on B-ALL blasts contrasted that on mature normal B-cells, where a decrease occurred in pro-B-ALL and c/pre-B-ALL samples at day 6 (paired t-test: p=.0485 and p<.0001, respectively) (Fig.1A, 2A).
In 24 paired blood/BM pre-treatment samples the percentage of CD20+ blasts was significantly higher in blood in c/pre-B-ALL (n=19: paired t-test: p=.0009), but not in pro-B-ALL (n=5: paired t-test: p=.095) (Fig. 1C, 2C). The significance levels were not consistently reached for the comparison of CD20-MFI. Nevertheless, we show that in 3/24 (12.5%) patients the percentage of CD20+ B-ALL blasts in BM did not reach the arbitrary cutoff of 20% whereas the matching diagnostic blood did.
Finally, CD20 expression levels from 25 BM and 30 pre-treatment blood samples and 38 blood samples after dexamethasone prephase from 54 patients were assessed (in total 93 samples). In further calculations we correlated MRD response values after one dose of Rituximab with the CD20 expression levels on blasts. In detail, the highest measured percentage value of %CD20 per patient in the group of MRD responders was compared to the highest measured %CD20 per patient in the group of MRD persisters. CD20 expression levels were significantly lower in 33 MRD persisters compared to 21 MRD responders (Fig 3, p=.0336). The difference was mainly attributable to a high frequency of MRD persisters in pro-B-ALL compared to c/pre-B-ALL (MRD persistence in pro-B-ALL 8/9 (89%) compared to 25/45 (56%) in c/pre-B-ALL).
Conclusion: We measured significant differences in CD20 expression levels on leukemic blasts (i) between pre-treatment blood and BM and (ii) between pre-treatment blood and blood after prephase in patients with c/pre-B-ALL challenging the conventional eligibility criteria for the CD20 targeted treatment. MRD responders tended to have higher CD20 expression levels compared to MRD persisters. Extension of the patient cohort is ongoing to confirm this observation. Furthermore, we will analyze the impact of 3 rituximab applications after induction phase II.
Ritgen:abbvie: Research Funding; Roche: Honoraria, Research Funding. Viardot:Gilead Kite: Consultancy, Honoraria; Roche: Consultancy, Honoraria; Pfizer: Consultancy, Honoraria; BMS: Consultancy, Honoraria; Amgen: Consultancy. Kneba:Roche: Consultancy, Honoraria; AbbVie: Consultancy, Honoraria. Goekbuget:Kite / Gilead: Consultancy; Celgene: Consultancy; Novartis: Consultancy, Other: Travel support, Research Funding; Pfizer: Consultancy, Other: Travel support, Research Funding; Amgen: Consultancy, Other: Travel support, Research Funding. Brüggemann:Incyte: Consultancy; Amgen: Consultancy, Research Funding, Speakers Bureau; PRMA: Consultancy; Affimed: Research Funding; Regeneron: Research Funding; Pfizer: Speakers Bureau; Roche: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.