Abstract
Background
Graft versus Host Disease (GvHD) still represents a major complication in allogeneic hematopoietic cell transplantation (HSCT) and a primary cause of non-relapse mortality.
GvHD, together with rejection and fungal infection, not only has been demonstrate to have a relevant impact in clinical outcome and quality of life but it is also associated with important direct costs during follow-up. Despite the relevance of this topic, so far there have been very few investigations and publications regarding the cost of HSCT in a long term perspective.
Methods
To address the evaluation of direct costs of GvHD, we retrospectively selected 15 patients who underwent HSCT in our Center for hematological diseases between 2009 and 2015. Patients were collected in 3 groups: no GvHD (Group A), chronic GvHD (Group B) and acute GvHD (Group C, 3/5 developed also chronic GvHD).
Those three groups were matched for known risk factors for outcome: conditioning regimens, GvHD prophylaxis, anti-infective prophylaxis, source of graft and donor selection according to Institutional policy.
We retrospectively collected parameters relevant for clinical course and direct costs: viral monitoring and reactivations, time of anti-infective prophylaxis and treatments, number of transfusions, days of hospitalization, number of outpatient clinical evaluations. GvHD treatment was also listed. All these parameters were monitored from discharge after HSCT procedure or after GvHD diagnosis, whichever occurred first. Finally all these parameters were compared between the three groups.
Results
Diagnosis at time of HSCT was acute myeloid leukemia (10 out of 15 cases); only one patient was transplanted for non-malignant disease. Five patients were transplanted from unrelated donor, four from matched siblings and six from haploidentical donors; peripheral blood was graft source in 14/15 and bone marrow in 1/15.
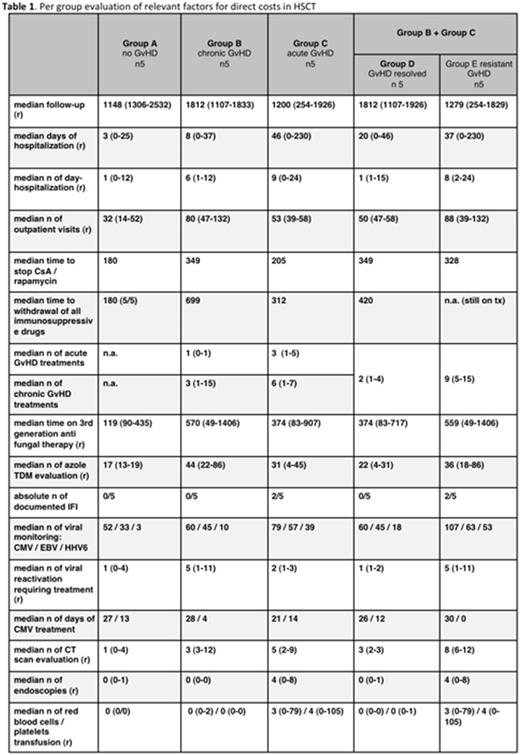
Per group evaluation of relevant factors for direct cost of HSCT is reported in Table 1.
In Group A (no GvHD) we documented lower re-hospitalization need, fewer out-patient clinical evaluations, shorter time of immunosuppressive treatment, lower incidence of infection and reduced need of anti-infective treatment.
In Group B (chronic GvHD) and Group C (acute GvHD +/- chronic GvHD) we documented higher re-hospitalization need, more out-patient clinical evaluations, longer time of immunosuppressive treatment (4/9 pts still under active treatment at a median follow-up of 49 months), higher incidence of infection and higher need of anti-infective treatment.
Differences are even more significant if patients from Group B and Group C are pooled and re-classified in Group D (complete GvHD resolution and withdrawal of immunosuppressive treatments) and Group E (pts with active GvHD still under immunosuppressive treatments at last FU).
Conclusions
Significant differences in events and direct costs are registered in 4-year follow-up period in patients with or without GvHD. Additionally, more relevant differences can also be documented in patients achieving a rapid response of GvHD and those requiring more than 2 lines of immunosuppressive treatments. These events computation represent the basis for direct costs calculation according to actual prices of drugs, examinations and procedures.
Impact of new therapies for GvHD prevention and treatment should be balanced according to direct costs evaluation in patients experiencing severe acute and chronic GvHD.
Marktel: GSK: Other: B-thalassemia gene therapy was developed by Fondazione Telethon and Ospedale San Raffaele and has been inlicenced by GSK that provides funding for the clinical trial, Research Funding. Ciceri: GSK: Other: B-thalassemia gene therapy was developed by Fondazione Telethon and Ospedale San Raffaele and has been inlicenced by GSK that provides funding for the clinical trial, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.