Abstract

Background: For patients with a first unprovoked venous thromboembolism (VTE), the optimal duration of anticoagulant therapy (AT) is a crucial clinical dilemma which has yet to be resolved . Choosing short-term (3-6 months) or indefinite AT, requires balancing the long-term risk of recurrent VTE when AT is discontinued, with the long-term risk of major bleeding (MB) from extended AT. Current guidelines suggest considering indefinite AT in all unprovoked VTE patients with non-high bleeding risk. This however, is a weak-evidence recommendation based on limited data, and no precise risk thresholds have been established to help guide treatment duration in this patient population. From an economic perspective, we aimed to identify thresholds of the risk of MB and recurrent VTE for which indefinite AT, as compared to stopping AT after initial short-term treatment, may be warranted.
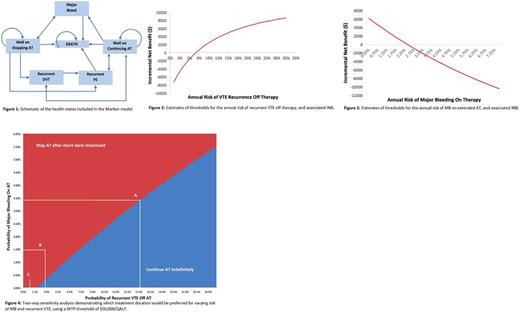
Methods: We constructed a Markov decision model of patients with a first unprovoked VTE who had completed at least 3-6 months of initial AT. The model adopted a lifetime horizon and a publicly-funded healthcare system perspective. Using a cycle length of one year, the model tracked recurrent VTE (DVT and/or PE), MB, and death from any cause [Figure 1]. For the base case, we considered patients aged 57 years, having a life expectancy of 30 years, annual risk of MB on Vitamin K Antagonists of 1.5%, annual recurrent VTE risk of 5% per year off therapy, case-fatality-rate (CFR) for MB of 11.3%, and CFR for recurrent VTE of 3.6%. We expressed our results as Incremental Net Benefit (INB) which incorporates costs, life-expectancy, quality-adjusted life-years (QALYs), and a willingness to pay (WTP) value. INB is the incremental benefit, expressed in monetary terms ($), of offering a patient treatment (indefinite AT) rather than the comparator (stopping AT). An INB > 0 favours the treatment, whereas an INB < 0 favours the comparator.
Results: For the base case analysis with assuming a decision-maker's WTP threshold of $50,000/QALY, indefinite AT was not justified (i.e. INB < 0) when the annual risk of recurrent VTE off therapy was less than 7.1% [Figure 2], or when the annual risk of MB exceeded 2.4% [Figure 3]. Furthermore, in a two-way sensitivity analysis [Figure 4], as the MB risk increased, so did the recurrent VTE risk threshold for which indefinite AT would be warranted. As illustrated through three hypothetical situations outlined in Figure 4; for a patient with an annual MB risk of 3.5% [scenario A], a recurrence risk of >15% would be required for indefinite AT to be favorable (i.e. INB > 0). Similarly, using a base case annual MB risk of 1.5% [scenario B], from an economic standpoint, the decision to offer indefinite AT would not be preferred for a patient in whom the risk of recurrence is 3%, but may be supported for a patient in whom the risk of recurrence is 10%. Lastly, for a patient with an annual recurrent VTE risk of < 1% [scenario C], continuing AT indefinitely would never be justified, irrespective of the risk of MB.
Conclusions/Implications: To the best of our knowledge, this is the first decision analysis of a hypothetical cohort of unprovoked VTE patients that identifies risk thresholds of MB and recurrent VTE to guide treatment duration. From an economic viewpoint, our analysis demonstrates that choosing indefinite AT in such patients may not be justified at the proposed risk thresholds. Furthermore, long-term follow up demonstrates that VTE recurs in less than 50% of such patients after stopping AT;thus, considering indefinite AT in all unprovoked VTE patients is an inefficient use of resources, and exposes a large proportion of patients to the unnecessary risks, burdens and costs of lifelong AT. Establishing risk thresholds, as achieved through our decision model, allows individualized treatment and helps guide patient-centered decision making. If validated and further optimized (as planned prior to the ASH), findings from our study could change clinical practice.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract