Abstract
Background Patients with acute leukemia who become refractory to chemotherapy have poor prognosis, with limited therapeutic options. Intensified conditioning and DLI have shown improved survival and good tolerability in this patient cohort in clinical trials, but have never been tested in randomized trials and real world data are scarce. We aimed at analyzing the impact of clinical and treatment-related factors on transplant outcome in an unselected, population-based cohort.
Methods Through the Chinese Blood and Marrow Transplantation Registry Group (CBMTRG), we identified 932 patients with refractory/relapsed acute leukemia receiving MSD or HID HCT during the period of 2003 to 2016. The median follow-up of survivors was 39 months.
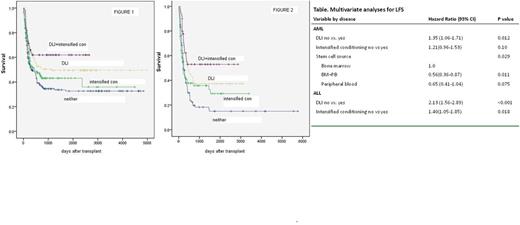
Results The 3-year leukemia free survival (LFS) rates were 40% for acute myeloid leukemia (AML) and 27% for acute lymphoblastic leukemia (ALL). In AML, LFS was not significantly improved with intensified conditioning alone (33% VS 41%, P=0.10), LFS was increased to 55% with the additional DLI (p=0.05, fig 1); In ALL, LFS was significantly improved with intensified conditioning alone (11% VS 30%, P=0.047), LFS was further increased to 51% with the additional DLI (p=0.004, fig 2). Multivariable analyses run separately in AML and ALL (Table). DLI was associated with a marked trend toward lower relapse, significantly lower NRM and higher LFS in AML and a significantly lower relapse and higher LFS in ALL in comparison to non-DLI, and no difference in ALL in terms of non-relapse mortality. Intensified conditioning was associated with a significantly lower relapse and higher LFS despite higher NRM in ALL in comparison to non-intensified conditioning; there was no impact of intensified conditioning in AML. In addition, HID was independently correlated with reduced relapse in both AML and ALL in comparison to MSD. Younger patient age was independently correlated with reduced NRM in both AML and ALL. Furthermore, in separate analyses in HID and MSD HCT, DLI had superior outcomes in both HID and MSD HCT while intensified conditioning only had influence on MSD outcomes; Similarly, the impact of patient age was only shown in MSD HCT. Besides, for AML patients with information on cytogenetics, poor cytogenetics resulted in higher relapse and lower LFS after MSD HCT in comparison to good or intermediate cytogenetics while there was no difference regarding cytogenetics in HID HCT.
Conclusions These data suggest that both DLI and intensified conditioning improved outcomes and are valid options in the treatment of refractory/relapsed acute leukemia, with the role of DLI more prominent and more extensive. HID had more GVL effect than MSD in some circumstances. By a population-based approach (the largest for HID group) from the real-world data, we were able to provide novel data on transplant outcomes in refractory/relapsed acute leukemia, applicable to routine clinical practice outside the setting of clinical trials.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.