Abstract
Introduction:
Only incremental gain in OS has been noted over the recent years for adults with ALL, when compared to the dramatic improvement in the pediatric and adolescent population. Though cytogenetics and molecular features primarily drive disease biology and OS, various socioeconomic factors influence receipt of optimal therapy and thereby OS. In this context, we utilized National Cancer Database (NCDB) to evaluate the impact of socioeconomic factors on OS in adult patients with ALL.
Methods:
NCDB Participant User File was used to extract patient-level data of adult patients (aged 18-80 years) diagnosed with ALL between 2003-2012. We excluded patients with unknown transplant or chemotherapy status and those who did not receive chemotherapy. Only patients treated in the reporting facility were included. Data abstracted include age, sex, race, Charlson comorbidity score, treatment facility type (academic vs. non-academic), median household income, insurance, and educational status. We performed multivariate logistic regression analysis to determine the association of these variables with OS.
Results:
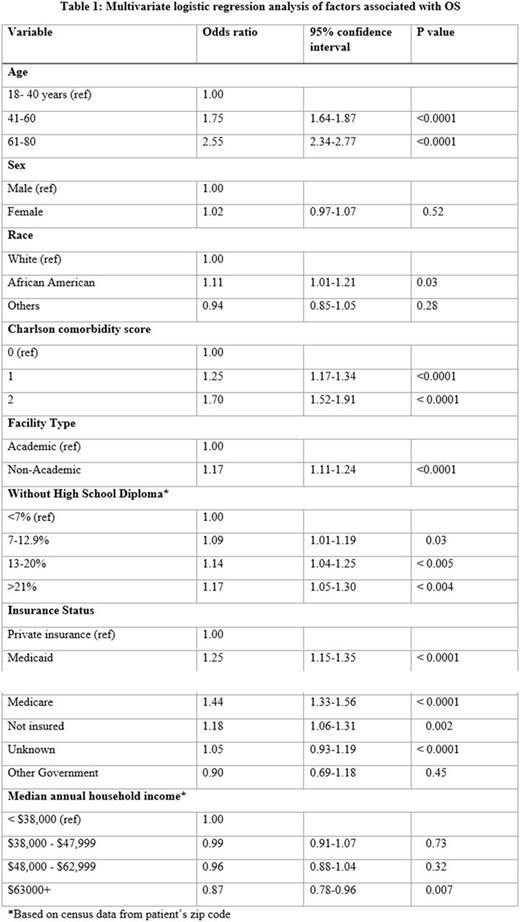
A total of 11,871 patients were included in the study. Median OS was 23 months (95% CI 22-24). In a multivariate analysis, patients who were older than 40 years (p<0.0001), African American (p<0.03), treated at non-academic facility (p<0.001), had higher Charlson comorbidity score (p<0.0001), lower educational status (p=0.004) and Medicaid/Medicare insurance (p<0.0001) or no insurance (p=0.002) were more likely to have inferior OS. Patients with median annual household income >$68,000 had superior OS (p=0.007) [Table 1].
Conclusion:
Our real-world data demonstrates an association between OS and socioeconomic factors such as race, treatment facility type, insurance, educational and income status. While the likelihood of lower OS in patients with advanced age and higher comorbidities are expected, the association with socioeconomic factors may indicate a possibility of health care disparity.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.