Abstract
Introduction: Bone disease is the most frequent complain of multiple myeloma (MM) and the major cause of comorbidity. IMWG established that more than one focal lesion on MRI and at least one bone lytic lesion detected on whole body low dose CT (WB-LDCT) or 18F-FDG PET/CT fulfill the criteria for bone damage requiring therapy. Most authors consider as bone disease only lytic bone lesions (LBL) caused by destruction of trabecular bone due to PCs proliferation that presents at CT an increased density value (Hounsifeld unit (HU)>0). However, lesions with fat density (HU <0) can also be detected on MM patients, sometimes representing the only detectable LBL. The aim of this study was to evaluate differences in densitometry, MRI characteristics and 18F-FDG metabolism in PET by use of PET/MRI of LBL identified by WB-LDCT in patients affected by newly diagnosed multiple myeloma (NDMM).
Methods: Eighteen patients (12 male and 6 female) affected by active MM, based on the IMWG criteria, that at diagnosis underwent both WB-LDCT and 18F-FDG-PET/MRI were included in the study. Every lytic bone lesion with diameter of at least 5 mm identified by WB-LDCT was characterized for dimensions and internal densitometry (negative or positive HU) by two expert radiologists. The same lesions were then evaluated by one radiologist and one nuclear medicine physician after PET/MRI analysis, registering T1w signal, T2w STIR (short tau inversion recovery) signal, DWI (diffusion weighted imaging) signal, mean ADC (apparent diffusion coefficient) value and SUV (standardized uptake volume) max value. PET/MRI was performed within 1 month from WB-LDCT.
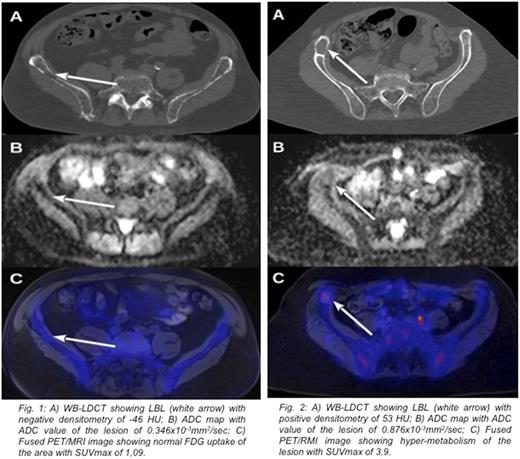
Results: A hundred thirtyfive lytic >5 mm diameter bone lesions were recognized by WB-LDCT in patients under study. Thirtyfive lesions (mean dimension 11,09 SD ± 1,5 mm) had a negative densitometry (mean -57,57 HU; SD ± 33,13 HU) showing high signal in T1w images, low signal in STIR and DWI sequences, while 100 lesions (mean dimension 17,36 SD ± 2,64) presented positive densitometry (mean 44,87 HU; SD ± 23,89) showing low T1w signal and high signal in STIR and DWI sequences. The first group presented low ADC values (mean 0,360x10-3 mm2/sec; SD ± 0,154) and low SUV max values (mean 1,69; SD ± 0,56), while the second group showed higher ADC values (mean 0,868x10-3 mm2/sec; SD ± 0,207) and SUV max values (mean 5,04; SD ± 1,94) (Fig. 1 and Fig.2). Mean ADC values and mean SUV max values between the two groups were statistically different (p value < 0,01). Eight patients presented positive and negative density LBL, 7 patients presented only positive density LBL and 3 patients presented only negative density LBL. In two patients of this latter group who did not start therapy, negative density LBL, became positive in conjunction with biochemical progression disease during the 12 months follow up. In terms of SUV and ADC a significant concordance was found between PET and MRI for both positive and negative densitometry LBL, (91% and 94%, respectively) considering a cut off value of SUV>2 and ADC>0,6 x10-3mm2/sec as abnormal. Finally, we showed a strong statistical correlation between positive densitometry LBL and ADC value >0,8 x10-3 mm2/sec, typical of focal lesion (58% vs. 2,86%, p<0,0001) and between positive densitometry LBL and SUV value >2 (92% vs. 2,86%, p<0,0001).
Conclusions: By measurement of internal densitometry, WB-LDCT differentiates two different patterns of lytic lesions: one characterized by fat replacement of trabecular bone (HU<0), likely expression of high osteoclastic activation, and one characterized by cell infiltration (HU>0). Both types of lesions can coexist in the same patient and were indicative of active disease, according to laboratory parameters. The observation that mean diameters of fatty LBL were significantly lower than that of proliferative LBL might suggest a particularly high cytokine/chemokine secreting PCs clone. Alternatively, fatty LBL might represent an early stage, which anticipates a massive infiltration by PCs. PET and MRI recognized only proliferative LBL, characterized by presence of pathological PCs within the lesion, whereas fat substitution of LBL led to a negative ADC and PET result. Then, if only PET/MRI had been evaluated, fatty LBL would have not been misleadingly considered as a proof of symptomatic disease. Especially in this subset of patients, WB-LDCT adds specific information, contributing to a proper definition of bone involvement in MM patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.