Abstract
Background
Myelodysplastic syndromes (MDS) are typically diseases of older adults. Children with MDS may have distinct molecular and clinical features or reflect a demographic continuum.
Method
We studied a cohort of 81 pediatric patients with various subcategories of myelodysplastic syndrome and acute myeloid leukemia with myelodysplasia-related changes. All subjects provided informed consent in compliance with the Declaration of Helsinki. Bone marrow and blood samples were collected. DNA was extracted from the patients' marrow and wherever possible germline DNA was obtained from selected CD3+ T cells. We designed a targeted sequencing assay to test a panel of 417 genes. The panel contain reported gene associated with MDS and IBMFs that need be differentiated. The average coverage of targeted region was 98.15%, and the average sequencing depth was 1000×.
Results
Clinical features ofpediatricmyelodysplastic syndrome
In the cohort, 51 (63%) were males and 30 (37%) females, with a median age of 6 years (range, 4months-18 years). According to the WHO 2008 criteria, 37 (46%) patients with refractory cytopenia of childhood (RCC), among them, 2 (3%) patients with RCUD, 30 (37%) RCMD, 2 (3%) RCMD-RS, and 3 (4%) MDS unclassifiable (MDS-U), 14 (17%) RAEB1, 16(20%) RARB2, 14 (17%) AML (MDS associated). Follow-up data was available for 73 (90%) subjects. Median follow-up for survivors was 18 months (range, 2-124). The 3-year and 5-year overall survival is 78% and 60%. The 3-year cumulative rate of leukemia transformation was 23.3%. According to the IPSSR, 2 (3%) patients were classified as very low risk group, 15 (21%) low risk , 14 (20%) intermediate risk, 15 (21%) high risk, and 24(34%) very high risk and the 3-year overall survival was 100%, 88%, 79%, 32% and 55% respectively (P=0.001). 29 (39.7%) subjects received bone marrow transplantation (BMT). the 3-year overall survival for patient with or without BMT was 96% and 45% (P=0.001). For patients with BMT, the IPSSR have no prognostic significance.
Patterns of molecular lesions
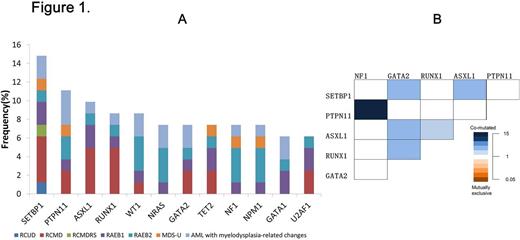
We found 397 mutations in 152 distinct genes with mutation loads varying from 10% to 100%. 17 (21%) subjects with 1 mutant gene, 17 (21%) with 2 mutant genes, 11 (14%) with 3 mutant genes and 14 (17%) with more than 3 mutant genes. 12 genes were mutated in greater than 5% of patients, namely SETBP1 15%, PTPN11 11%, ASXL1 10%, RUNX1 9%, WT1 9%, NRAS 7%, GATA2 7%, TET2 7%, NF1 7%, NPM1 6%, GATA 1 6%,, U2AF1 6%. The distribution of gene mutations (>5%) observed in the entire study set was mirrored within the disease categories (Figure 1A).
Compared to SETBP1 wildtypesubjects, SETBP1 mutated subjects were significantly associated with abnormal karyotype (P=0.019). Compared to PTPN11 wildtypesubjects, PTPN11 mutated subjects were significantly associated with younger than 6-year old and poor survival (3-year OS: 46% vs. 26%, P=0.031). However, WT1 or NPM1 mutated subjects were significantly associated with elder than 6-year old (P=0.002). GATA2 mutation was enriched for SETBP1 mutation (P=0.012, OR=7.33, 95%CI: 1.28-42.02), ASXL1 mutation (P=0.013, OR=14, 95%CI: 2.223-88.16), and RUNX1 mutation (P<0.001, OR=17.75, 95%CI: 2.68-117.7). More detailed association between different gene mutations is shown in Figure 1B.
Conclusion
Compared with gene mutation landscape in adult MDS, children with MDS have distinct gene mutation characteristics. Our study indicates some interesting association between different genes. The further identification has the potential to advance understanding of the pathogenesis of pediatric myelodysplasia.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.