Abstract
Background: Immune thrombocytopenia (ITP) is a heterogeneous disorder of immune dysregulation of T and autoreactive B cells leading to immune mediated destruction of platelets due to eventual loss of immune tolerance against platelet epitopes. Whether intensification regimens like Rituximab improve sustained platelet response (SR) across different lines is unclear.
Methods: A retrospective review of three hundred sixty-two patients of thrombocytopenia seen between Jan 1990 to June 2016 across three rural community practices across southeastern NM was performed. Eighty-eight patients with chronic liver disease and or drug related thrombocytopenia were excluded from the statistical analysis. Fisher's exact test was used to test the association of treatment and response in both primary and secondary ITP. International working group (IWG-2009) classification was used to assess response criteria. (SR) was defined as a platelet count of >50,000 per cubic millimeter six months after treatment.
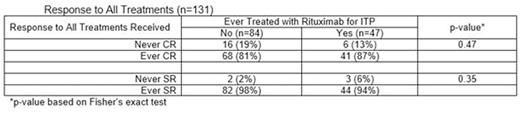
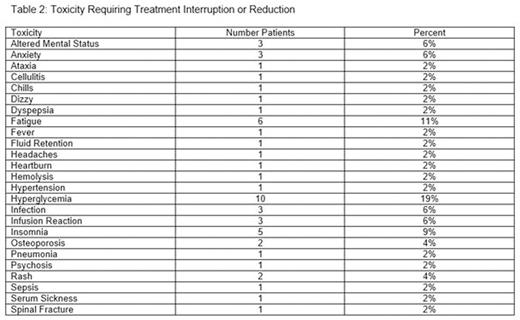
Results: Two hundred thirty-three patients (64%) had primary ITP 41 (11%) had secondary ITP. Median age of diagnosis was 61 and median platelet on diagnosis was 90 (0-148). Of the 274 patients included in this analysis, 143 ITP patients (52%) were followed by observation alone and 131 (48%) received treatment. Sixty-six (24%) patients received second line treatment and further 41 (15%) patients received third line treatment. Complete remission (CR) was achieved in 68% in first line. Sixty-one percent patients had a CR with Prednisone in first line as compared to 84% with dexamethasone (p=0.15). Forty-seven (17%) of all ITP patients received Rituximab (across multiple lines of treatment). Twenty percent of patients who achieved CR/PR in first line had received IVIg. Rituximab was used in 9%,39% and 34% of first, second and third lines of treatment respectively. Across all lines of treatment Rituximab was not associated with a higher CR (p=0.47) or SR (p=0.35) (Table 1). Fifteen percent of patients had toxicity requiring interruption of Rituximab including 1 patient with sepsis. Hyperglycemia, insomnia were the three most common toxicities seen in 19%, 11% patients overall (Table 2).
Conclusion: Rituximab use across all lines of treatment was not associated with a higher CR or SR rate in our dataset. The higher than expected Response rates may be due to inclusion of other intensification treatments like IVIg. The use of Rituximab however is limited in real world rural practices especially in the first line setting possibly partly due to insurance denials and cost. Its use seems more common in subsequent lines of treatment. Other ways to intensifying therapy in first line should be evaluated in prospective clinical trials like use of IVIg with or without the use of Rituximab and whether upfront intensive treatment avoids earlier recurrence need to be studied.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.