Abstract
Therapy-related acute myeloid leukemia/myelodysplastic syndrome (t-AML/MDS) arise after cytotoxic chemotherapy and/or radiotherapy administered for a prior neoplasm and have a dismal outcome (median survival of 8 months in the largest series published including 306 patients (pts), Smith, Blood 2003). Recent registry data suggested a continued increase in survival in AML (Derolf, Blood 2009) and we wondered whether this was also observed in the setting of t-AML/ MDS.
All pts with a t-AML/MDS diagnosed and/or treated for their prior neoplasm at Gustave Roussy Cancer Center between July 1986 and 2016 were included in this retrospective study. Data regarding pts' demographics, primary diagnosis and treatment, latency time, cytogenetic, treatment and outcome were collected. The diagnosis of t-AML/MDS was based on the WHO 2016 classification. t-AML were classified based on cytogenetic results as favorable, intermediate and adverse according to international classification, t-MDS based on IPSS score as favorable (Low, Int-1) and adverse (Int-2 and High).
428 pts were analyzed. The median age at diagnosis of t-AML/MDS was 56.4 years with a female predominance (60%). 224/428 (52.3%) pts had t-AML, 204/428 (47.7%) t-MDS. The most common primary malignancies were breast cancer (24%), non-Hodgkin lymphoma (15%), Hodgkin lymphoma (HL) (9%) and ovarian cancer (9%). Occurrence of t-AML/MDS following HL represented 26.6% of t-AML/MDS cases between 1986-96 comparing to 4 % between 2006-16 whereas breast cancer rose from 16% to 45%. Prior treatments included chemotherapy alone in 137/428 pts (32%), radiotherapy alone in 61 pts (14%) and both in 230 pts (54%).
At diagnosis of t-AML/MDS, 295 pts (69%) were in complete remission (CR) of their prior neoplasm, 29 (7%) had a stable and 104 (24%) a progressive disease. Median interval between primary cancer and t-AML/MDS was 5 years (4.3 and 5.7 years for t-AML and t-MDS respectively, (p=0.03)). Furthermore, delay to develop t-AML/MDS after radiotherapy alone was longer compare to chemotherapy or both (6.1, 5.1 and 4.3 years, respectively (p=0.0087)). In the t-AML subgroup, 47% of pts presented unfavorable cytogenetic (including complex karyotype (20%) and 11q23 abnormalities (16.9%)), 26% intermediate and 26% favorable cytogenetic (core binding factor mutations (12.7%), t(15;17) (13.3%)). In the t-MDS subgroup, 78% of pts were considered adverse; complex karyotype, chromosome 7 and 5 abnormalities were found in 40.8%, 46.7% and 28.9% respectively. Pts received intensive chemotherapy (including 41 allografts), low dose chemotherapy (including 74 treatments with hypomethylating agents) and best supportive care in 42%, 24% and 34% respectively.
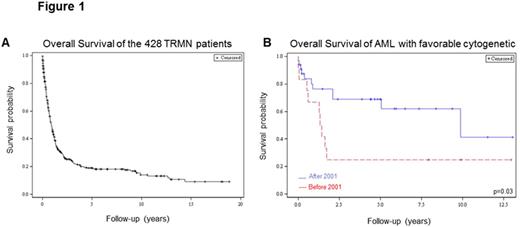
The median overall survival (OS) was 10.6 months and the 5-year survival was 19.1% (Figure 1A). The 5-year OS of patients in CR of their prior neoplasm was 25.5% compared to 3.65 and 0% for pts with progressive and stable disease, respectively (p<0.001). 5-year OS was not statistically different between t-AML and t-MDS subgroups (23.3% vs 13.5%) and between hematologic or oncologic malignancies as primary diagnosis (12.6% vs 21.1%). Pts with favorable risk t-AML had better 5-year survival compared with patients with intermediate or unfavorable risk disease (55.5% vs 20% vs 12.1% respectively, p<0.001). In addition, favorable t-MDS was associated with better 5-year OS compared to adverse t-MDS (34.9% vs 6.6%, p<0.001). We next compared OS of pts diagnosed for their t-AML/MDS after or before July 2001. A trend for better OS for pts diagnosed in the last 15 years was observed (21.5% vs 15.1%, p=0.39). Interestingly outcome of t-AML patients with favorable subtype significantly improved over the last 15 years (68.8% vs 25%, p=0.03, Figure 1B) which was not the case for other cytogenetic subgroups and for t-MDS, especially pts with adverse prognosis (4.6% vs 3.9%, p=0.92). Pts who received allograft had a trend for better OS in the last 15 years (52.8% vs 21.5% p=0.2).
t-AML/MDS are still associated with a low 5-year OS (19.1%) but our results are upper than previous publications. However, a significant improvement of survival in favorable t-AML was observed during the past 30-years, with a trend for pts who benefit from allograft. In addition to improve treatment for t-MDS pts, detection of the disease at the earliest stage is a real challenge to improve their survival.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.