Abstract
Introduction: Acalabrutinib and ibrutinib are Bruton's tyrosine kinase (BTK) inhibitors, which have revolutionized the treatment of B-cell lymphoma/leukemias such as mantle cell lymphoma (MCL) and chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) in frontline or relapsed refractory setting. Outcomes of patients with MCL and/or CLL who progressed on ibrutinib therapy are poor. Few reports have shown that ibrutinib resistant patients develop specific BTK mutations which confer resistance. We present the clinical and molecular data on patients with follicular lymphoma (FL) who have progressed on either ibrutinib based regimen or on acalabrutinib.
Methods: We selected FL patients enrolled in clinical studies at our institution between 2013 and 2015 who discontinued acalabrutinib or ibrutinib for various reasons. Survival post ibrutinib discontinuation was calculated. We performed whole-exome sequencing on pre and post treatment (paired) samples of 3 FL patients (progressed on ibrutinib) using DNA extracted from formalin fixed paraffin embedded tissue samples. Library preparation and capture were performed using Agilent's SureSelect XT Human All Exon V4. Following capture the enriched libraries were pooled and sequenced in two Illumina HiSeq4000 lanes using a 75nt paired-end configuration.
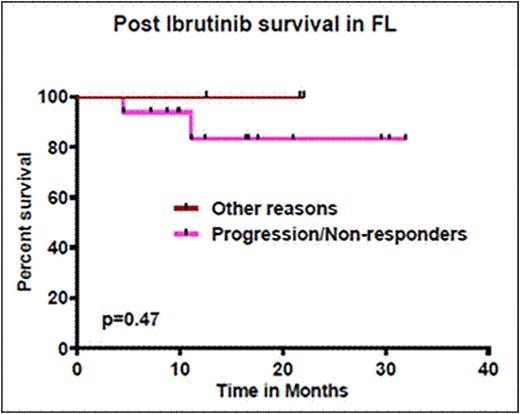
Results: Twenty of 55 patients discontinued treatment with BTK inhibitors; 5 came off from single agent acalabrutinib in relapsed refractory FL (RR-FL) while 15 came off from ibrutinib based regimen (4 as a single agent in RR-FL while 11 were treated with ibrutinib and rituximab in the frontline setting). These patients discontinued BTK inhibitor treatment, after a median of 2.8 months (range 0.9-22 months). Patients who received frontline ibrutinib (n=11), discontinued at a median of 2.8 months (0.9-22 months); previously treated patients discontinued BTK inhibitors at a median of 2.8 months (1.4-7.6 months). The reasons for discontinuation were as follows - 14 disease progression (3 on acalabrutinib and 11 on ibrutinib; 1 of them developed classical Hodgkin lymphoma), 2 non-responders (1 acalabrutinib and 1 ibrutinib) and 4 for other reasons (1 due to fatigue on acalabrutinib, 3 due to ibrutinib - 1 elevated liver enzymes, 1 asymptomatic atrial fibrillation another lost to follow up). Pre-treatment characteristics of the 16 patients who either progressed or were nonresponders to BTK inhibitors were - median age 59 years (range 41-75), 69% had stage 4 disease, 31% had FLIPI score of 3 or 4 and median LDH levels were 457 IU/L (range 290-754). Median follow up after discontinuation for all patients was 14.4 months (0-32 months). Eighteen patients (90%) were alive at the time of last follow up and 2 (10%) have died. Median survival (figure 1) of patients according to the causes of discontinuation was: not reached for both group of patients, those with other causes and those in progressive disease and/or non-responders.
All 16 patients who progressed or not responded were treated with additional therapies. At the time of last follow up, 10/16 (62%) were responding to subsequent therapy - 5/10 (62%) achieved CR on lenalidomide-based therapies, 4/10 (40%), responded to chemoimmunotherapy and 1 patient responded to venetoclax-bendamustine and rituximab with CR. None were treated with PI3K inhibitors. WES studies showed EZH2 Y646 mutations in 2 of 3 FL patients in both pre and post treatment samples. Comparison of pre and post treatment samples on 3 patients showed multiple non-recurrent variants (2-12 per patient) in several genes in the post-treatment samples. These included DNMT3A R882H, NOTCH2 A3D and MLL E765G, all of which were noted in the post treatment sample of the patient that progressed to CHL. None of the other detected variants have been implicated in cancer. Of note, none of the samples showed BTK mutations despite adequate coverage.
Conclusions: In contrast to other B-cell malignancies such as CLL and MCL, we observed that almost all FL patients who progressed on BTK inhibitors were salvageable by alternate therapies. Absence of BTK gene mutations in paired samples of 3 patients who progressed on ibrutinib suggests alternate mechanisms of drug resistance.
Outcomes of patients with follicular lymphoma after discontinuing acalabrutinib and/or ibrutinib based regimen according to the cause of discontinuation
Outcomes of patients with follicular lymphoma after discontinuing acalabrutinib and/or ibrutinib based regimen according to the cause of discontinuation
Wang:Janssen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Acerta Pharma: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Juno Therapeutics: Research Funding; Onyx: Research Funding; Kite Pharma: Research Funding; Asana BioSciences: Research Funding; Celgene: Research Funding; Pharmacyclics: Research Funding; BeiGene: Research Funding. Fayad:Seattle Genetics: Consultancy, Research Funding. Oki:Novartis: Research Funding. Westin:Spectrum: Membership on an entity's Board of Directors or advisory committees; Chugai: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees; ProNAi: Membership on an entity's Board of Directors or advisory committees. Fowler:Gilead: Research Funding; Jannsen: Consultancy, Research Funding; Infinity: Consultancy, Research Funding; Roche: Consultancy, Research Funding; Celgene: Consultancy, Research Funding; TG Therapeutics: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.